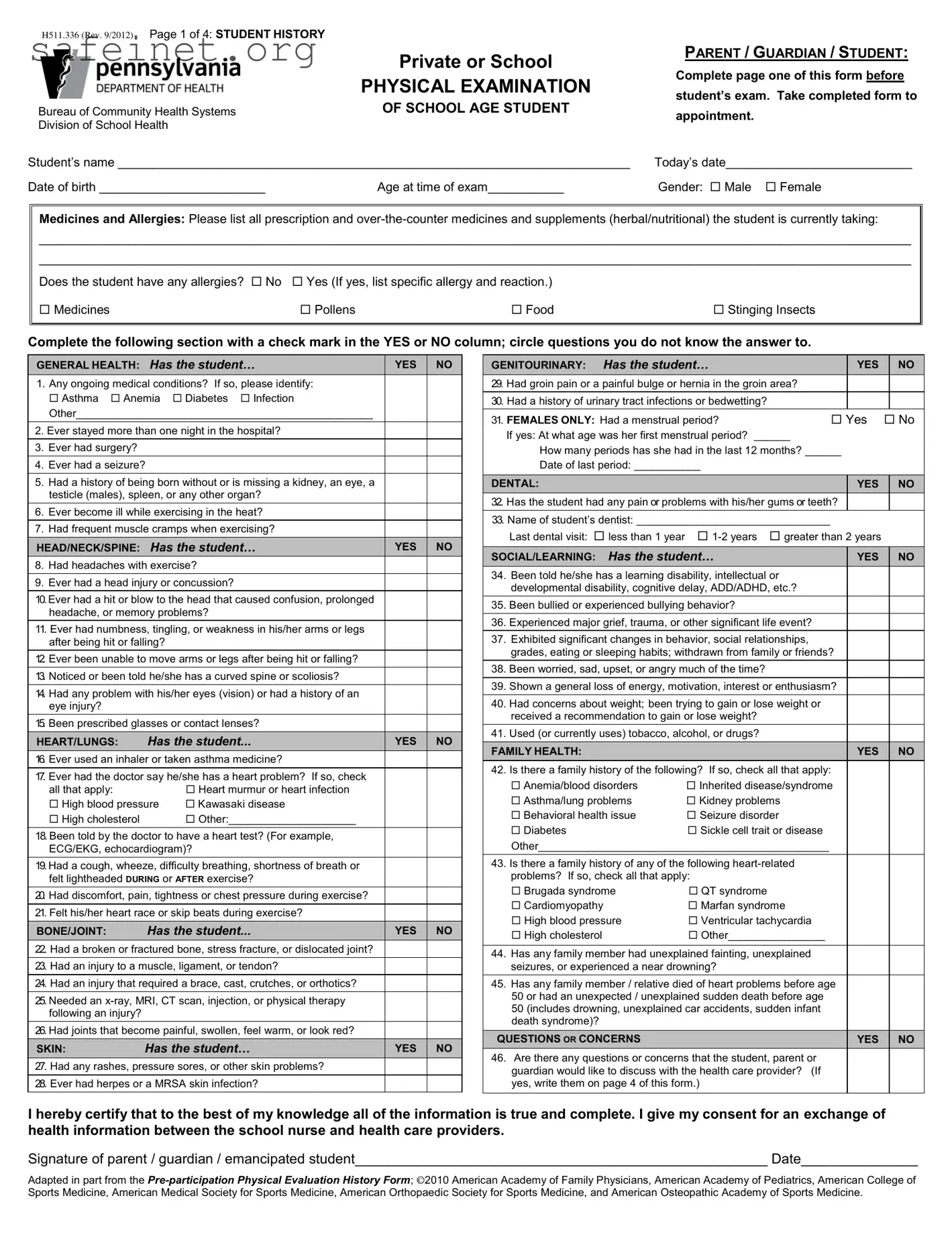
What is the purpose of the Physical Exam form?
The Physical Exam form is designed to gather important health information about a student before their examination. It allows parents or guardians to provide details about the child's medical history, current medications, allergies, and social or learning concerns. This information helps healthcare providers assess the student's health and identify any specific needs during the exam.
Who is responsible for completing the form?
The form should be completed by the parent, guardian, or emancipated student. They need to fill out the first page before the student's health appointment. It’s important to provide as much accurate information as possible to ensure the healthcare provider understands the student’s health history.
What information is required in the “Medicines and Allergies” section?
This section asks for a list of all prescription and over-the-counter medications, supplements, or herbal/nutritional products the student is currently taking. Additionally, it inquires about any known allergies the student may have, including the type of allergy and the reaction experienced. Filling this out helps avoid any potential adverse reactions during the examination.
Why is the student’s health history important?
The health history is crucial because it provides context for the physical exam. By reviewing the student's past medical conditions, surgeries, and injuries, the healthcare provider can better anticipate and address the student’s health needs during the examination. It can also guide decisions related to sports participation and other activities.
What happens if something is marked as “abnormal” on the form?
If any portion of the Physical Exam form indicates an abnormal finding, the healthcare provider will typically discuss these concerns with the parent or guardian. They may recommend further tests or referrals to ensure the student's health is appropriately monitored and managed.
Is it necessary to keep the information in the form updated?
Yes, it's vital to keep the information current. If there are any changes in the student’s health, medications, or allergies after the physical exam, those details should be updated in the student’s health records. This ensures all healthcare providers involved are aware of the student's latest health status and can provide appropriate care.
How is the Physical Exam form used by the school?
Once completed, the Physical Exam form is submitted to the school nurse and is kept on file. It helps the school monitor the health and wellbeing of students. The information can also assist in making decisions regarding health needs, accommodations, or interventions at school, especially for students with ongoing health concerns.