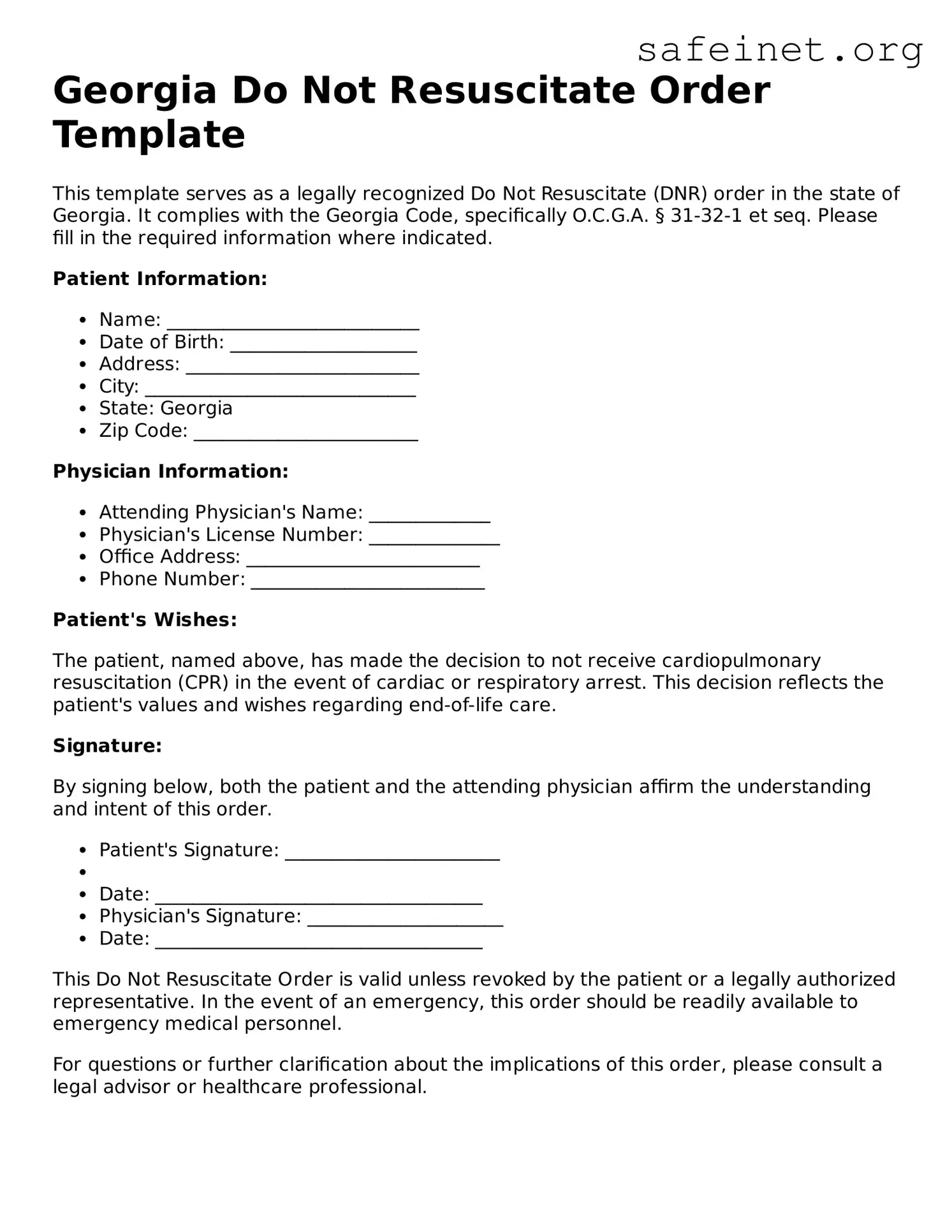
Georgia Do Not Resuscitate Order Template
This template serves as a legally recognized Do Not Resuscitate (DNR) order in the state of Georgia. It complies with the Georgia Code, specifically O.C.G.A. § 31-32-1 et seq. Please fill in the required information where indicated.
Patient Information:
- Name: ___________________________
- Date of Birth: ____________________
- Address: _________________________
- City: _____________________________
- State: Georgia
- Zip Code: ________________________
Physician Information:
- Attending Physician's Name: _____________
- Physician's License Number: ______________
- Office Address: _________________________
- Phone Number: _________________________
Patient's Wishes:
The patient, named above, has made the decision to not receive cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. This decision reflects the patient's values and wishes regarding end-of-life care.
Signature:
By signing below, both the patient and the attending physician affirm the understanding and intent of this order.
- Patient's Signature: _______________________
-
- Date: ___________________________________
- Physician's Signature: _____________________
- Date: ___________________________________
This Do Not Resuscitate Order is valid unless revoked by the patient or a legally authorized representative. In the event of an emergency, this order should be readily available to emergency medical personnel.
For questions or further clarification about the implications of this order, please consult a legal advisor or healthcare professional.