What is a Florida Do Not Resuscitate Order (DNRO)?
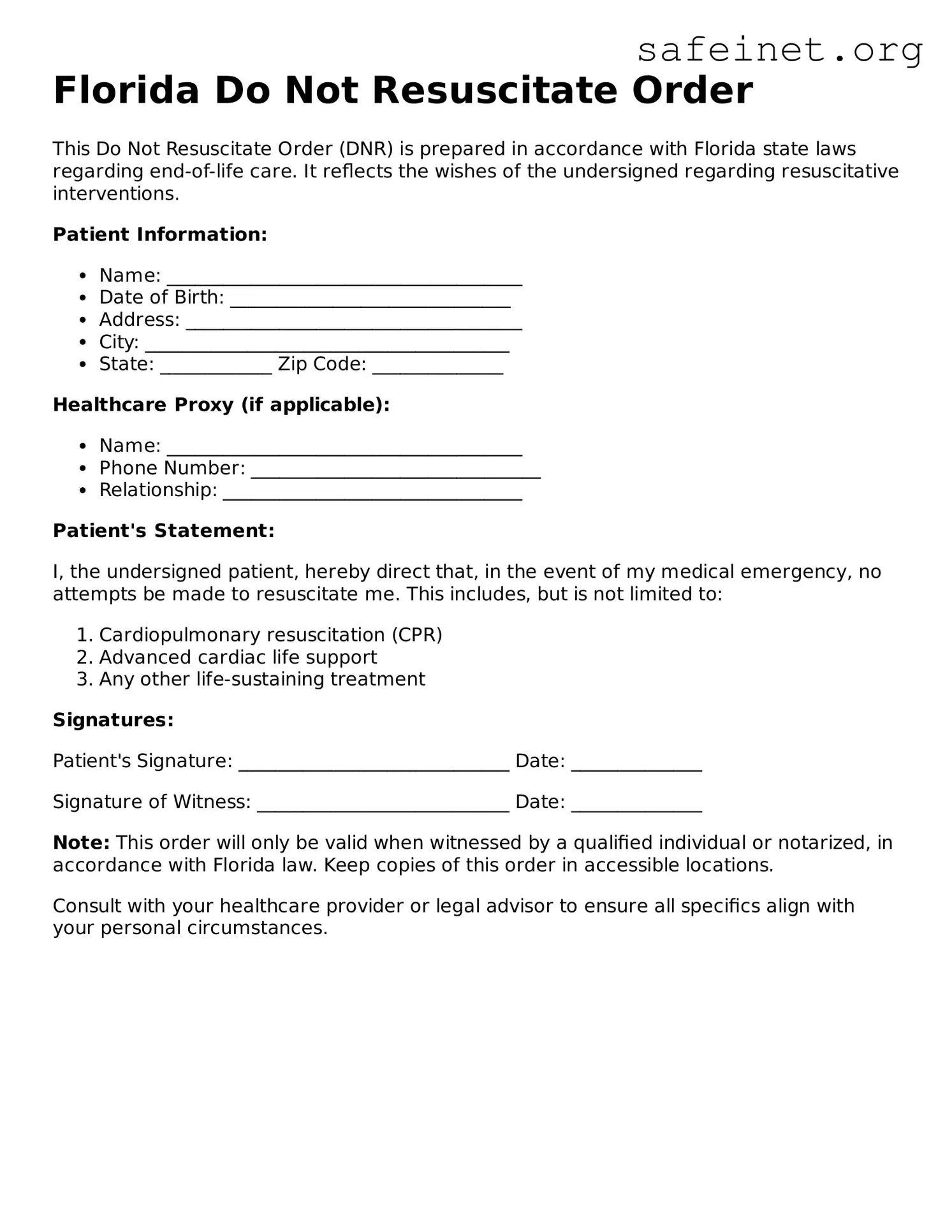
A Florida Do Not Resuscitate Order is a legal document that informs medical personnel that a person does not wish to receive cardiopulmonary resuscitation (CPR) or other lifesaving measures in the event of cardiac or respiratory arrest. It serves to honor the patient's wishes regarding end-of-life care.
Who can create a DNRO in Florida?
Any adult or legally authorized representative can create a DNRO in Florida. This includes individuals with a clear understanding of their medical condition and the implications of the order. Guardians and health care proxies can also make the decision on behalf of a patient.
How is a DNRO executed?
To execute a DNRO, the individual must complete the official Florida DNRO form. The form must be signed by the patient or their representative and a physician. The physician's signature indicates that the patient has made an informed decision about their end-of-life care.
Where should the DNRO be kept?
It is essential to keep the DNRO in a location that is easily accessible, such as on the refrigerator or in a medical file. Additionally, individuals should carry a copy in their wallet or purse. Medical personnel must be able to see this document quickly in emergency situations.
Does a DNRO apply in all medical situations?
No, a DNRO specifically applies to situations where a patient is in cardiac or respiratory arrest. It does not prevent other forms of medical treatment or intervention that may be necessary for the patient’s health or comfort.
Can a DNRO be revoked?
Yes, a DNRO can be revoked at any time by the patient or their representative. To revoke a DNRO, simply destroy the document and communicate the change to appropriate medical personnel. A new DNRO can also be completed if the patient's wishes change.
Is a DNRO the same as a living will?
No, a DNRO is not the same as a living will. While a living will provides guidance on a person's preferences for medical treatment and end-of-life care, a DNRO specifically addresses wishes related to resuscitation efforts in emergency situations.
Are there any specific requirements for the physician's signature on the DNRO?
Yes, the physician must be licensed to practice medicine in Florida. The physician's signature confirms that they have discussed the DNRO with the patient and that the patient understands the implications of such an order.
Will my DNRO be recognized in other states?
Florida's DNRO may not be automatically recognized in other states. It's advisable to check the local laws and regulations in the state where the person plans to travel or live. Some states have their own forms that may be necessary to ensure compliance.
What should I do if emergency personnel arrive and my DNRO is not visible?
If emergency personnel arrive and cannot see the DNRO, they will be legally obligated to provide lifesaving treatment, including CPR. It’s important to inform family members and caregivers about the DNRO so that they can present it in an emergency.