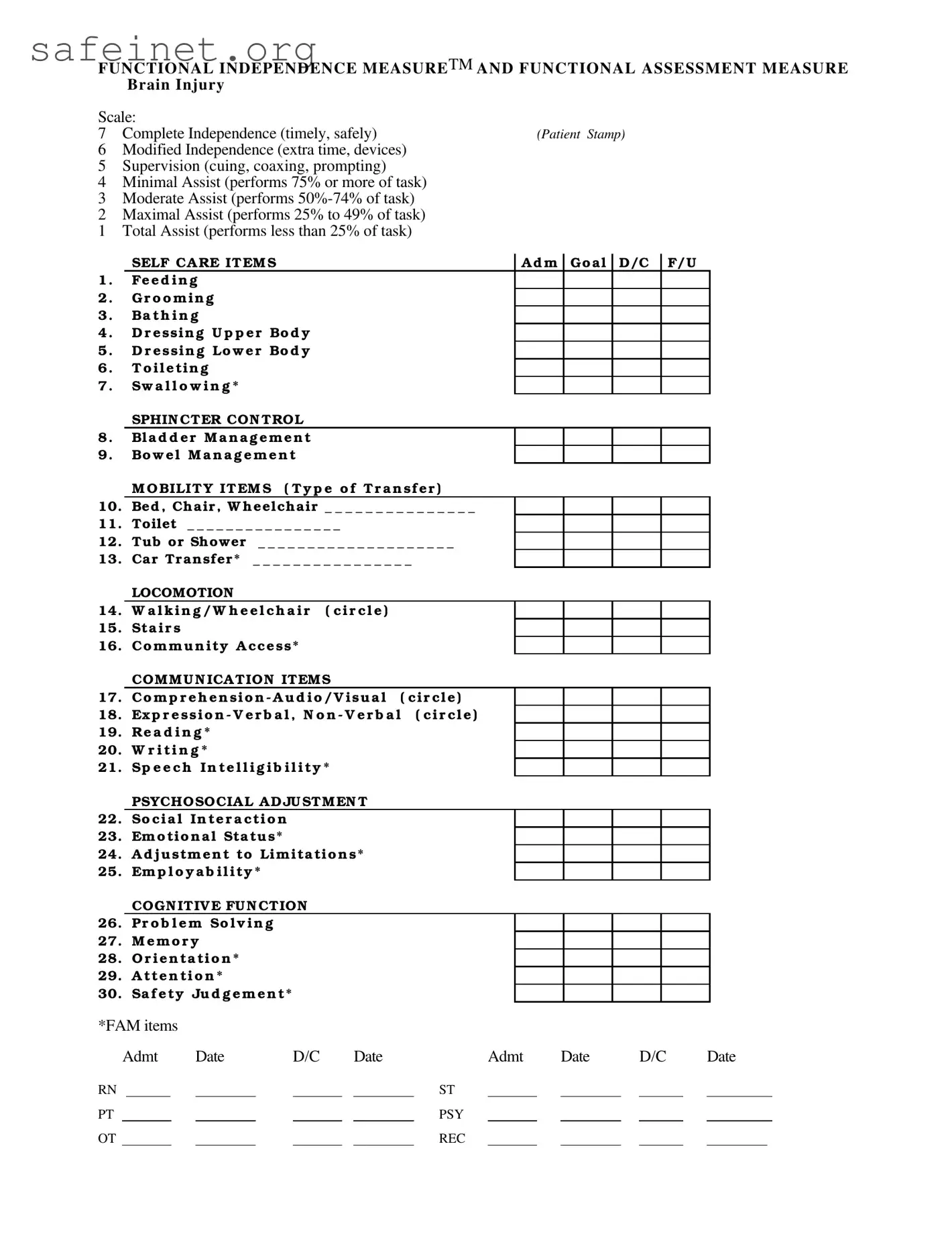
FUNCTIONAL INDEPENDENCE MEASURETM AND FUNCTIONAL ASSESSMENT MEASURE
BRAIN INJURY
Scale: |
|
7 Complete Independence (timely, safely) |
(Patient Stamp) |
6Modified Independence (extra time, devices)
5Supervision (cuing, coaxing, prompting)
4Minimal Assist (performs 75% or more of task)
3Moderate Assist (performs 50%-74% of task)
2Maximal Assist (performs 25% to 49% of task)
1Total Assist (performs less than 25% of task)
|
SELF CA RE IT EM S |
|
A d m |
Go a l |
D/C |
F/U |
1 . |
Fe e d i n g |
|
|
|
|
|
|
2 . |
G r o o m i n g |
|
|
|
|
|
|
3 . |
Ba t h i n g |
|
|
|
|
|
|
4 . |
D r e ssin g U p p e r Bo d y |
|
|
|
|
|
5 . |
D r e ssi n g Lo w e r Bo d y |
|
|
|
|
|
6 . |
T o i l e ti n g |
|
|
|
|
|
|
7 . |
Sw a l l o w i n g * |
|
|
|
|
|
|
|
SPHIN CTER CON TROL |
|
|
|
|
|
8 . |
Bl a d d e r M a n a g e m e n t |
|
|
|
|
|
9 . |
Bo w e l M a n a g e m e n t |
|
|
|
|
|
|
M O BILIT Y IT EM S ( T y p e o f T r a n sf e r ) |
10. |
Bed , Ch air , W h eelch air _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ |
|
|
|
|
11. |
Toilet _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ |
|
|
|
|
12. |
Tub or Shower |
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ |
|
|
|
|
13. |
Car Tr ansfer * |
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ |
|
|
|
|
|
LOCOMOTION |
|
|
|
|
|
|
14. |
W a l k i n g / W h e e l c h a i r |
( c i r c l e ) |
15.Sta i r s
16.Co m m u n i ty A cce ss*
|
COM M U N ICA TION ITEM S |
17. |
Co m p r e h e n si o n - A u d i o / V i su a l ( ci r cl e ) |
18. |
Ex p r e s s i o n - V e r b a l , N o n - V e r b a l ( ci r cl e ) |
19.Re a d i n g *
20.W r i t i n g *
21.Sp e e c h I n t e l l i g i b i l i t y *
PSYCHOSOCIA L A D JU STM EN T
22.So ci a l In te r a cti o n
23.Em o tio n a l Sta tu s*
24.A d j u stm e n t to Lim ita tio n s*
25.Em p l o y a b i l i ty *
COGN ITIV E FU N CTION
26.Pr o b l e m So l v i n g
27.M e m o r y
28.O r i e n ta ti o n *
29.A tte n ti o n *
30.Sa f e ty Ju d g e m e n t*
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
*FAM items |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Admt |
Date |
|
D/C |
|
Date |
|
Admt |
Date |
|
D/C |
|
Date |
RN |
|
|
|
|
|
|
|
ST |
|
|
|
|
|
|
|
|
PT |
|
|
|
|
|
|
|
PSY |
|
|
|
|
|
|
|
|
OT |
|
|
|
|
|
|
|
REC |
|
|
|
|
|
|
|
|