What is the purpose of the Express Scripts Androgel Prior Authorization Form?
The Express Scripts Androgel Prior Authorization Form is designed to help patients acquire the necessary approval for Androgel, a medication often prescribed for low testosterone levels. This form ensures that the prescribing physician provides essential patient and treatment information that meets Express Scripts' criteria. It plays a crucial role in facilitating timely access to medication for patients who require it, while also adhering to the policies of various health insurance plans.
What information is required to complete the form?
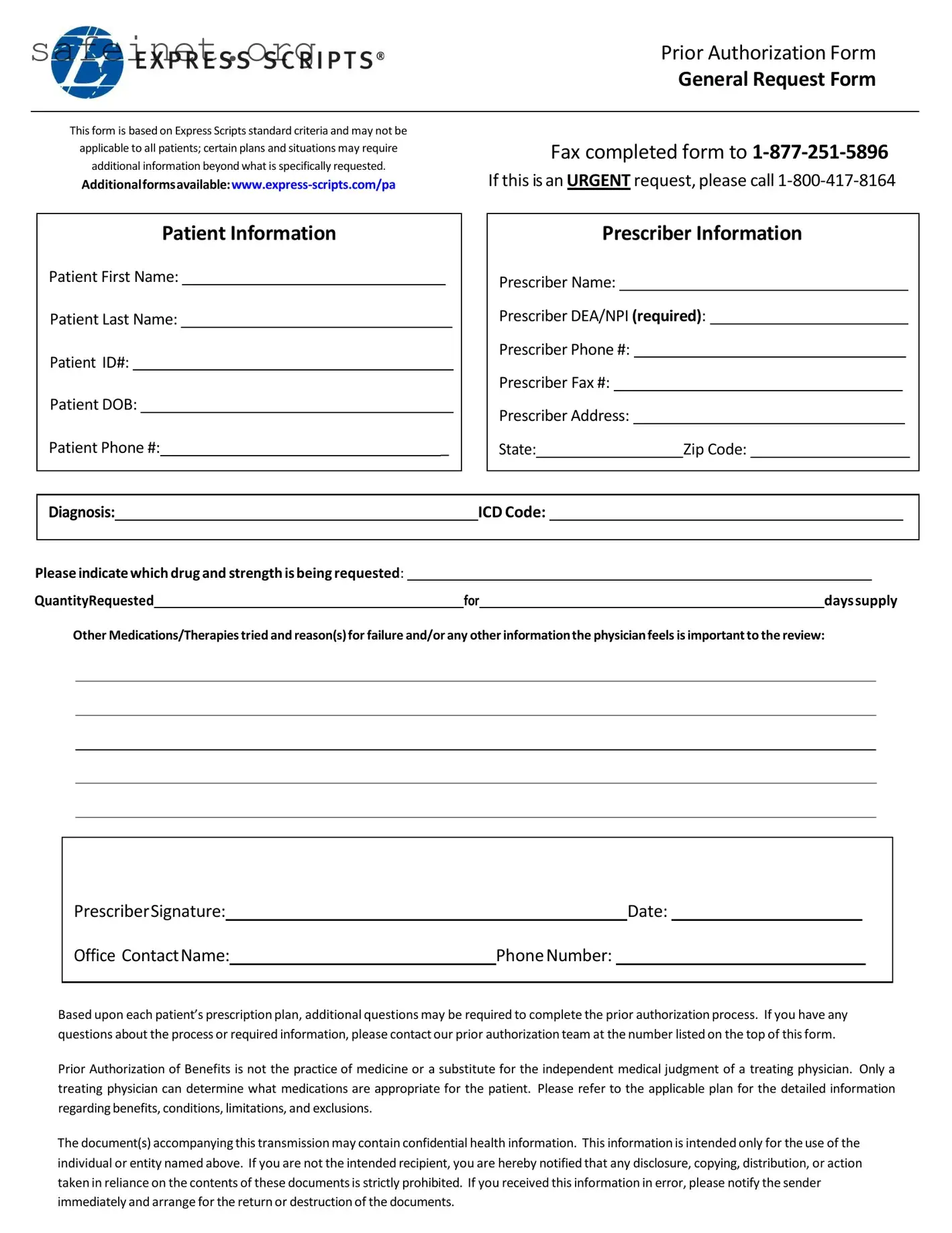
To complete the Prior Authorization Form, you will need to provide detailed information about both the patient and the prescriber. This includes the patient’s full name, identification number, date of birth, and contact number. Similarly, details about the prescriber are needed, including their name, DEA or NPI number, contact information, and address. Additionally, the form requests information regarding the patient’s diagnosis, the specific drug and strength requested, the quantity needed, and any previous medications or therapies attempted, including reasons for failure. It’s important to ensure that this information is accurate and complete to facilitate the approval process.
How do I submit the completed form?
Once the form is filled out, it needs to be submitted to the prior authorization team at Express Scripts. You can fax the completed form to 1-877-251-5896. If the request is urgent, you are encouraged to call 1-800-417-8164 instead. This ensures that your request receives timely attention and consideration, which can be critical for ongoing patient care.
What happens after I submit the Prior Authorization Form?
After submission, the prior authorization team will review the information provided. They may contact the prescriber for additional details or clarification as required by the specific insurance plan. The team’s goal is to make a determination on the authorization request based on the stated needs and medical necessity. Depending on the plan and the decision made, you will be notified of the outcome, which could include approval, denial, or a request for further information.
Who should I contact if I have questions about the process?
If questions arise during the completion or submission of the Prior Authorization Form, you can reach out to the prior authorization team directly at the number listed on the top of the form. They can provide guidance on required information or clarify any aspects of the process to ensure that you successfully navigate the prior authorization system. Remember, patient care is the priority, and support is available to help facilitate this process.