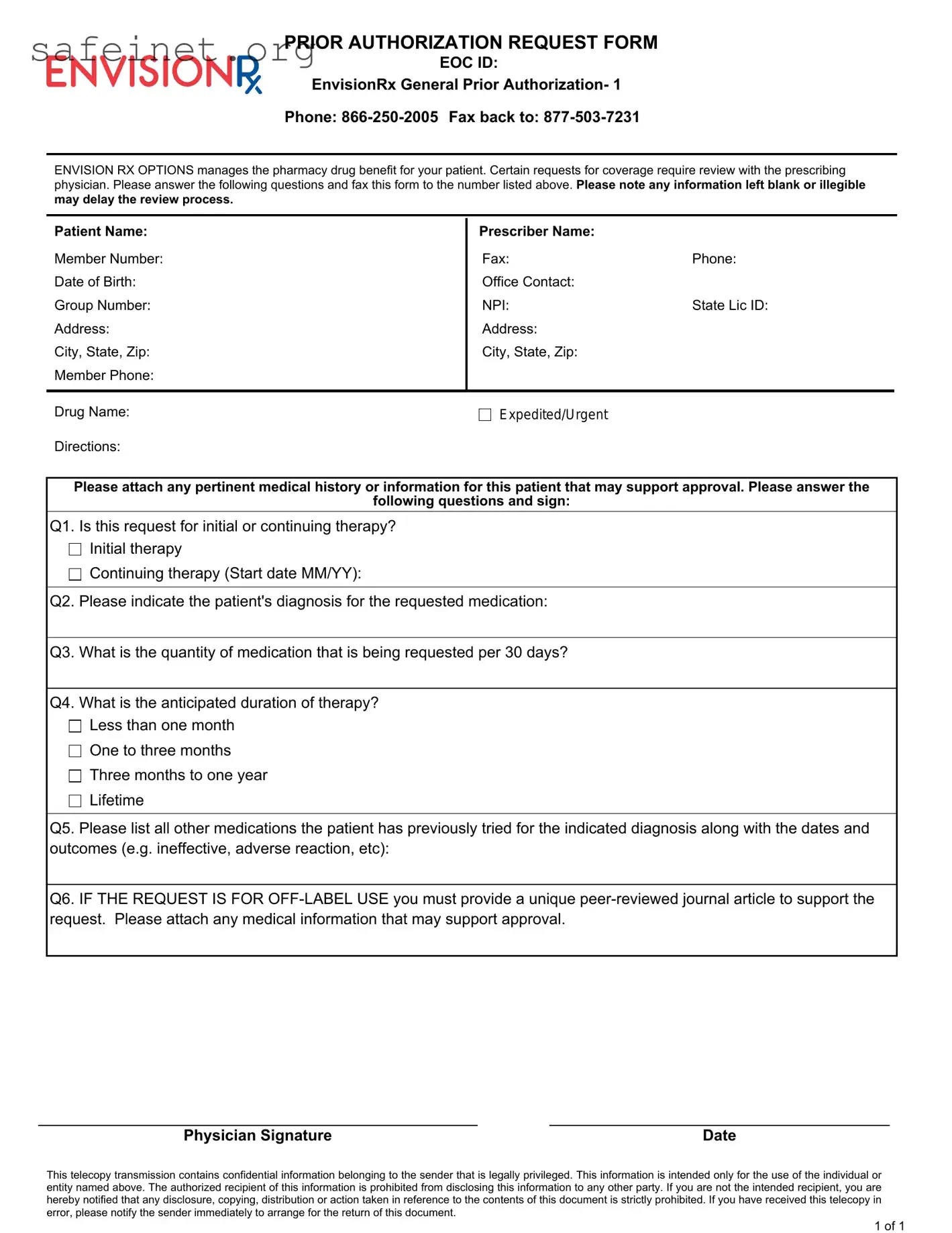
What is the Envision Rx Prior Auth form used for?
The Envision Rx Prior Auth form is utilized to request coverage for specific medications that require pre-approval. It ensures that the medication is medically necessary for the patient, based on the prescribing physician's assessment.
Who needs to fill out the Prior Auth form?
This form must be completed by the prescribing physician. It includes important information regarding the patient's medical history, diagnosis, and the requested medication.
What information is required to complete the form?
To fill out the form adequately, the prescriber must provide details such as the patient’s name, member number, date of birth, diagnosis, anticipated duration of therapy, and any previous medications tried. It’s crucial to answer all questions clearly to avoid delays.
What happens if I leave information blank or it is illegible?
Leaving any section blank or submitting an illegible form may cause delays in the review process of the prior authorization request. It is essential to ensure that all information is completed accurately and clearly.
How should the completed form be submitted?
Once completed, the form should be faxed to the designated number: 877-503-7231. It's important to retain a copy for your records and confirm that the fax has been sent successfully.
What is considered initial therapy versus continuing therapy?
Initial therapy refers to the first time the patient will be receiving the medication, while continuing therapy indicates that the patient has been on the medication previously. Indicating the correct option helps the review process in understanding the patient's treatment history.
What should I include if the request is for off-label use?
If the medication is being requested for off-label use, it is required to attach a unique peer-reviewed journal article that supports the request. This information is crucial in evaluating the appropriateness of the off-label use.
What is the anticipated duration of therapy?
Anticipated duration can vary based on the patient’s specific condition and treatment plan. Typical options include less than one month, one to three months, three months to one year, or lifetime therapy. Clearly indicating this will assist in the review process.
Can I appeal if the prior authorization is denied?
If a denial occurs, there can be an appeal process in place. The prescriber may need to submit additional documentation or clarification to support the request. Specific guidelines for appeals can usually be found within the policy or from the Envision Rx contact details provided.
How do I contact Envision Rx if I have questions about the form?
If you have questions regarding the prior authorization form or need assistance, you can contact Envision Rx directly at 866-250-2005. They can provide clarification and further guidance on completing and submitting the form.