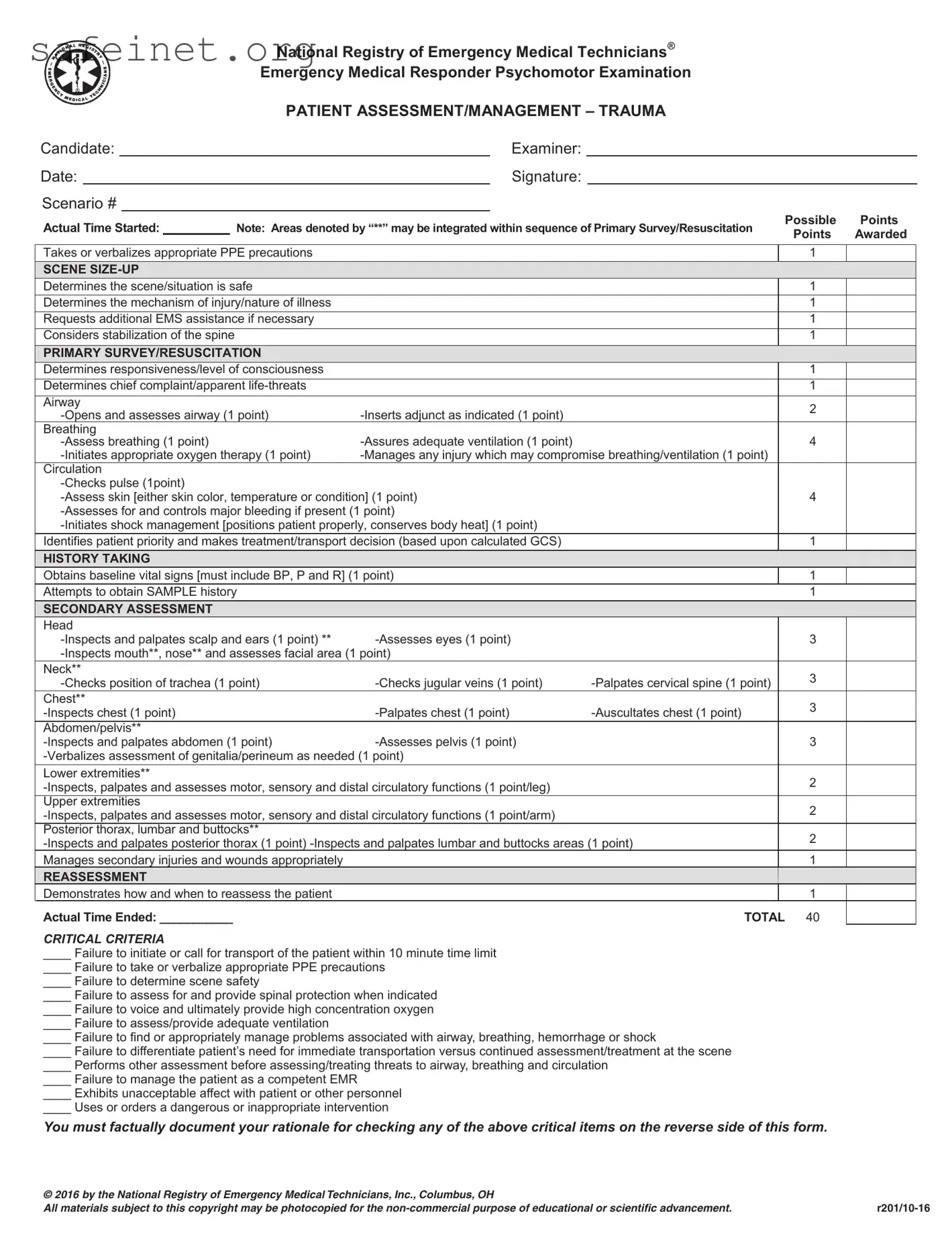
What is the purpose of the EMT Trauma Assessment form?
The EMT Trauma Assessment form is designed to guide emergency medical responders in assessing and managing trauma patients. It helps ensure that all essential procedures are followed systematically, allowing for a thorough evaluation and appropriate treatment of injuries. By using this form, medics can track critical information about the patient's condition and the care provided during an emergency situation.
What are the key components of the Primary Survey/Resuscitation section?
The Primary Survey/Resuscitation section focuses on three main areas: airway, breathing, and circulation. First, responders must open and assess the airway, and if necessary, insert an adjunct to maintain it. Next, they evaluate the adequacy of ventilation and may initiate oxygen therapy. Lastly, checking the pulse, skin condition, and controlling any significant bleeding are essential to assess the patient's circulation. This rapid assessment helps identify life-threatening conditions that require urgent attention.
How important is scene safety in the trauma assessment process?
Scene safety is paramount in emergency medical situations. Responders must ensure that the environment is secure before approaching the patient. This includes evaluating for potential hazards, determining the mechanism of injury, and requesting additional help if needed. Neglecting scene safety can put not only the patient's life at risk but also the lives of responders and bystanders.
What does the SAMPLE history acronym stand for?
The SAMPLE acronym is a tool used for obtaining crucial information about the patient. It stands for Signs and Symptoms, Allergies, Medications, Past medical history, Last oral intake, and Events leading up to the incident. Collecting this information can help responders better understand the patient's condition and tailor their treatment accordingly.
Why is reassessment necessary during the management of a trauma patient?
Reassessment is vital to monitor the patient's condition and the effectiveness of the treatments administered. It helps responders identify any changes in the patient's status, allowing for timely interventions when necessary. By performing regular reassessments, medics can improve patient outcomes and respond to emerging issues that may arise during transport or on scene.
What are some critical criteria that can indicate failure during the assessment process?
Several critical criteria can signify potential failure in addressing a trauma patient’s needs. These include failing to initiate timely transport of the patient, neglecting to assess or protect the airway, breathing, and circulation, or not providing appropriate oxygen if required. Other issues might include not recognizing the need for spinal protection or managing the patient improperly. Addressing these criteria is essential for ensuring the best possible care in emergencies.
How should documentation be handled following the use of the EMT Trauma Assessment form?
Documentation must be thorough and factual. It should include details regarding the patient's condition, the treatments applied, and any critical decisions made during the assessment. If any critical criteria are indicated on the form, responders are required to document their rationale for checking those items. Accurate documentation is crucial not only for legal purposes but also for continuous patient care and quality improvement in emergency medical services.