What is the purpose of the E/M Audit form?
The E/M Audit form serves as a structured tool for healthcare providers to evaluate and document the complexity and quality of patient visits. It helps ensure that the medical decision-making, history, and examination details align with the coding chosen for billing and reimbursement. This process is vital to maintain compliance with regulations and to optimize reimbursement for services provided.
How should I complete the form for each patient encounter?
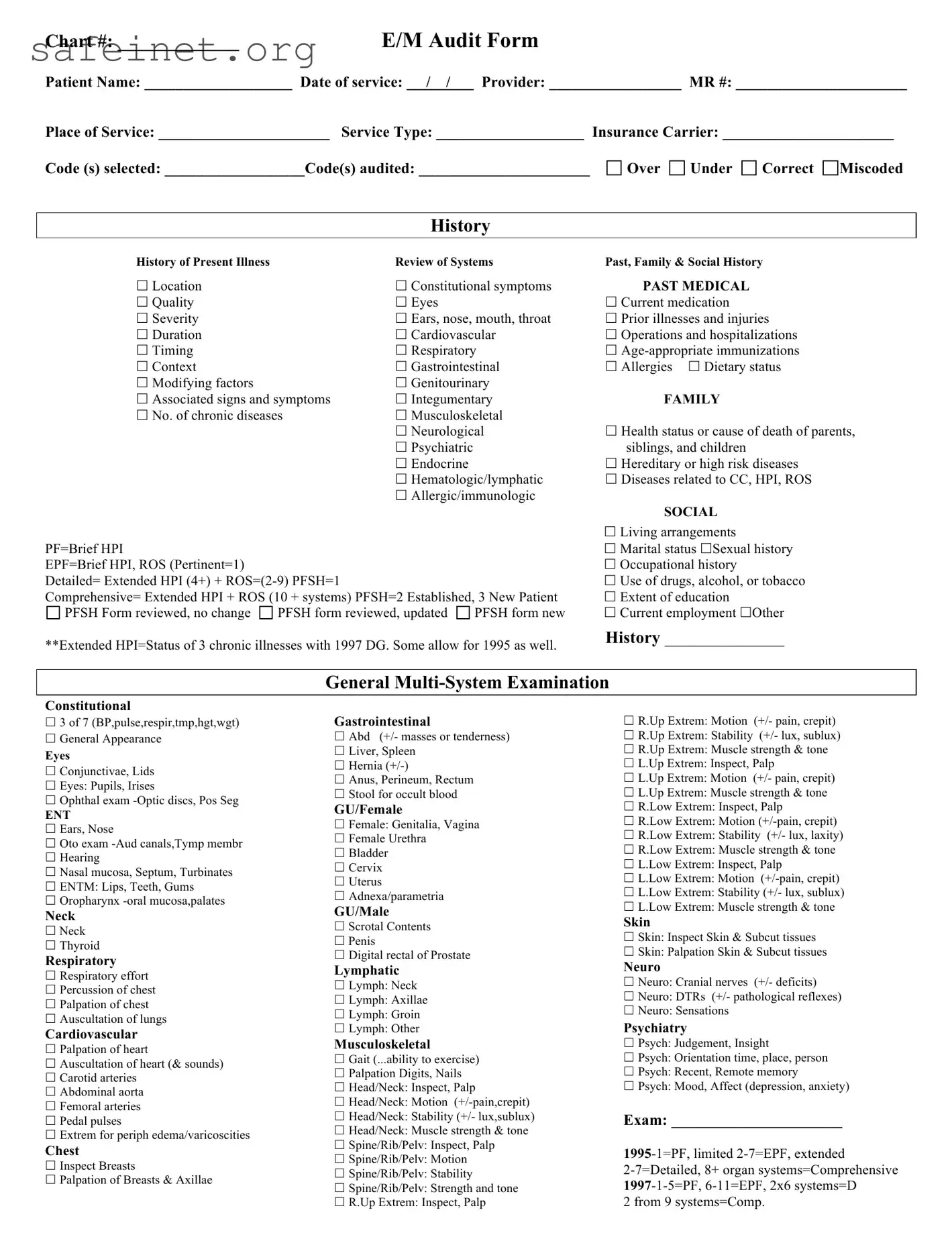
To complete the form accurately, start by populating the basic patient information, including chart number, patient name, date of service, and provider details. Carefully document all relevant data pertaining to the patient's history, examination, and medical decision-making. Ensure that you check all applicable boxes concerning the history and examination components. Remember to select the correct codes that best reflect the services rendered, as this is critical for proper billing.
What is meant by 'History' in the context of the E/M Audit form?
The 'History' section evaluates the information gathered about the patient's current condition, past medical history, and relevant family and social backgrounds. It assesses the depth of the History of Present Illness (HPI), Review of Systems (ROS), and Past, Family, & Social History (PFSH). Each category is essential for creating a comprehensive view of the patient's health and informs the medical decision-making process.
What kind of details should be included in the ‘Examination’ section?
In the 'Examination' section, document findings from the patient’s physical examination in an organized manner. This includes constitutional checks (like vital signs), detailed examinations of various body systems (e.g., eyes, cardiovascular, gastrointestinal, musculoskeletal), and necessary neurological assessments. Aim to provide a thorough yet concise overview of significant findings that contribute to diagnosing the patient’s condition.
How does the form classify different levels of medical decision-making?
The E/M Audit form categorizes medical decision-making into various levels based on the complexity of diagnoses, amount and complexity of data to review, and the associated risks involved. These levels can range from minimal to high, helping auditors assess the appropriateness of the codes assigned based on the services rendered. Understanding these levels assists providers in evaluating the necessity of their actions and documentation.
What are the implications of incorrect coding on this form?
Incorrect coding can lead to several issues, including delayed or denied reimbursement from insurance companies. It may also expose healthcare providers to audits or compliance investigations. Overcoding can result in fines or penalties, while undercoding could mean lost revenue for services rendered. Accurate and thorough completion of the E/M Audit form helps mitigate these risks.
What should I do if I find that I have made an error on the form?
If you discover an error on the E/M Audit form, it's essential to address it promptly. Cross out the incorrect information, write the correct details clearly, and initial the change. Additionally, make a note of the change in the patient’s chart to ensure that there is a clear record of what was amended. This transparency will aid in any future reviews or audits.
Can the form be used for both established and new patients?
Yes, the E/M Audit form is suitable for both established and new patients. However, it is important to note that the criteria and documentation requirements may differ slightly for each category. When assessing new patients, providers typically need to gather more comprehensive information compared to established patients, as the latter will already have a medical history documented.
How do insurance companies utilize the information gathered in the E/M Audit form?
Insurance companies use the information from the E/M Audit form to determine if the billed services align with the documented patient care. They evaluate the documentation for accuracy, completeness, and appropriateness of the chosen codes. This assessment helps the insurers decide whether the care provided warrants payment and verifies that it adheres to established healthcare guidelines.
What resources can assist providers in learning more about properly using the E/M Audit form?
Providers can access a variety of resources to enhance their understanding of the E/M Audit form. These include coding manuals, online courses, webinars, and professional organizations that offer training on E/M coding guidelines. Collaboration with billing specialists and attending workshops can also provide practical knowledge and insights into effectively utilizing the form, leading to better compliance and more accurate billing practices.
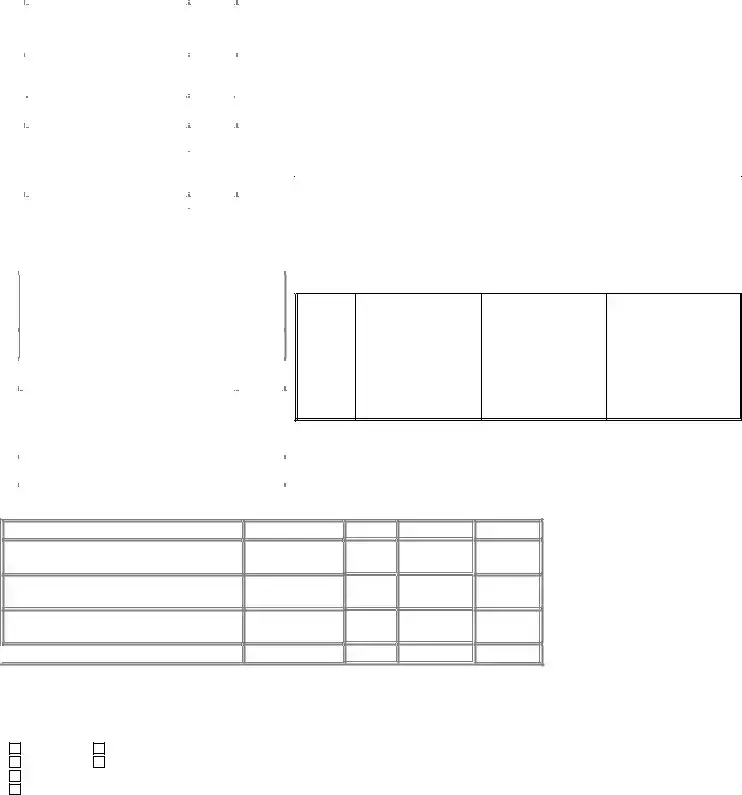

 MDM Level=2 out of 3
MDM Level=2 out of 3