What is a Do Not Resuscitate Order (DNR) form?
A Do Not Resuscitate (DNR) order is a legal document that specifies a person’s wish not to receive cardiopulmonary resuscitation (CPR) in the event of a cardiac arrest or when breathing stops. This order comes into play during emergencies, directing medical personnel to refrain from attempting resuscitation procedures. It is an essential part of advance care planning, allowing individuals to express their desires about life-saving measures when they are unable to communicate them themselves.
Who should consider a DNR order?
Individuals with serious, life-limiting illnesses or those who are nearing the end of life might find a DNR order particularly relevant. Additionally, anyone who has strong feelings regarding medical interventions at the end of their life should consider this order. Engaging in these discussions with family and healthcare providers can help clarify personal values and preferences regarding medical care.
How does someone obtain a DNR order?
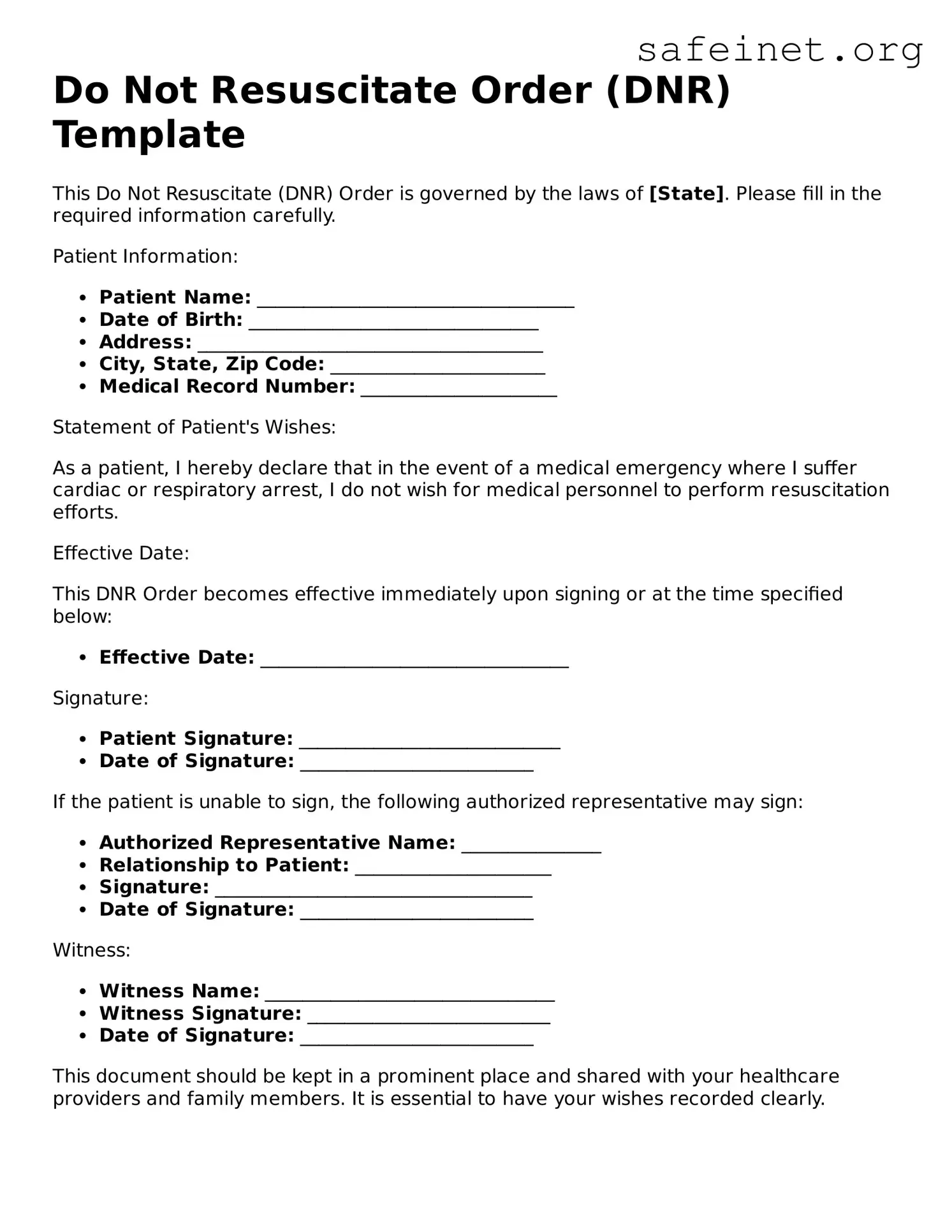
To obtain a DNR order, a conversation with a healthcare provider is vital. This discussion typically involves outlining personal health conditions and discussing preferences about potential medical interventions. Based on this conversation, the healthcare provider can complete the necessary documentation. Some states also offer official DNR forms that can be filled out and signed. It is important to ensure that the form is properly executed according to local laws.
Will a DNR order affect other types of medical care?
No, a DNR order specifically addresses resuscitation efforts during cardiac arrest or respiratory failure. It does not influence other forms of medical treatment, such as pain management, comfort care, or life-extending procedures. Patients with a DNR order can still receive comprehensive medical care in accordance with their wishes and best interests.
What if a person changes their mind about their DNR order?
If someone chooses to change their mind about their DNR order, they can do so at any time. This can involve notifying healthcare providers and family members, as well as formally rescinding the order by canceling the document. It is advisable to create a new DNR order that explicitly states the desire to override the previous one. Open communication about the change ensures that everyone involved understands the current wishes.
Can family members override a DNR order?
A DNR order is intended to reflect the wishes of the individual who signed it. Family members typically cannot override a legally executed DNR order unless there are specific legal grounds to challenge it. Therefore, having discussions with family members about end-of-life wishes can help prevent confusion or conflict during critical moments.
Do DNR orders have to be recognized in all healthcare settings?
Generally, DNR orders should be recognized across various healthcare settings, including hospitals, nursing homes, and emergency medical services. However, local laws and regulations can differ, which is why it’s essential to ensure that the DNR is photographed or copied and shared with all relevant parties—this includes carrying a copy in a wallet or keeping one easily accessible at home.
How do emergency medical services handle DNR orders?
Emergency medical services (EMS) are required to honor valid DNR orders. However, they may need to confirm that the order is valid and that it meets all legal requirements. Having a clearly visible DNR order, such as a bracelet or card, can expedite this process. It is crucial to ensure that the DNR order is up-to-date and compliant with local regulations, so that EMS personnel are aware of the patient’s wishes upon arrival.
What considerations should be taken into account when discussing a DNR order with loved ones?
When discussing a DNR order with loved ones, focus on open and honest communication. It’s vital to express why this order aligns with personal values and preferences. Sharing fears, concerns, and hopes regarding end-of-life care can foster understanding and support. Emphasizing the importance of individual autonomy can help family members come to terms with these decisions, making the conversation both meaningful and respectful.
Is a DNR order needed if someone has a living will?
A living will outlines an individual’s preferences regarding medical treatment in situations where they cannot express their wishes. While it can include directives about resuscitation, a separate DNR order is often still necessary to ensure that emergency services are informed of the individual’s wishes. Therefore, it is advisable for individuals to have both documents in place to provide comprehensive guidance regarding their care.