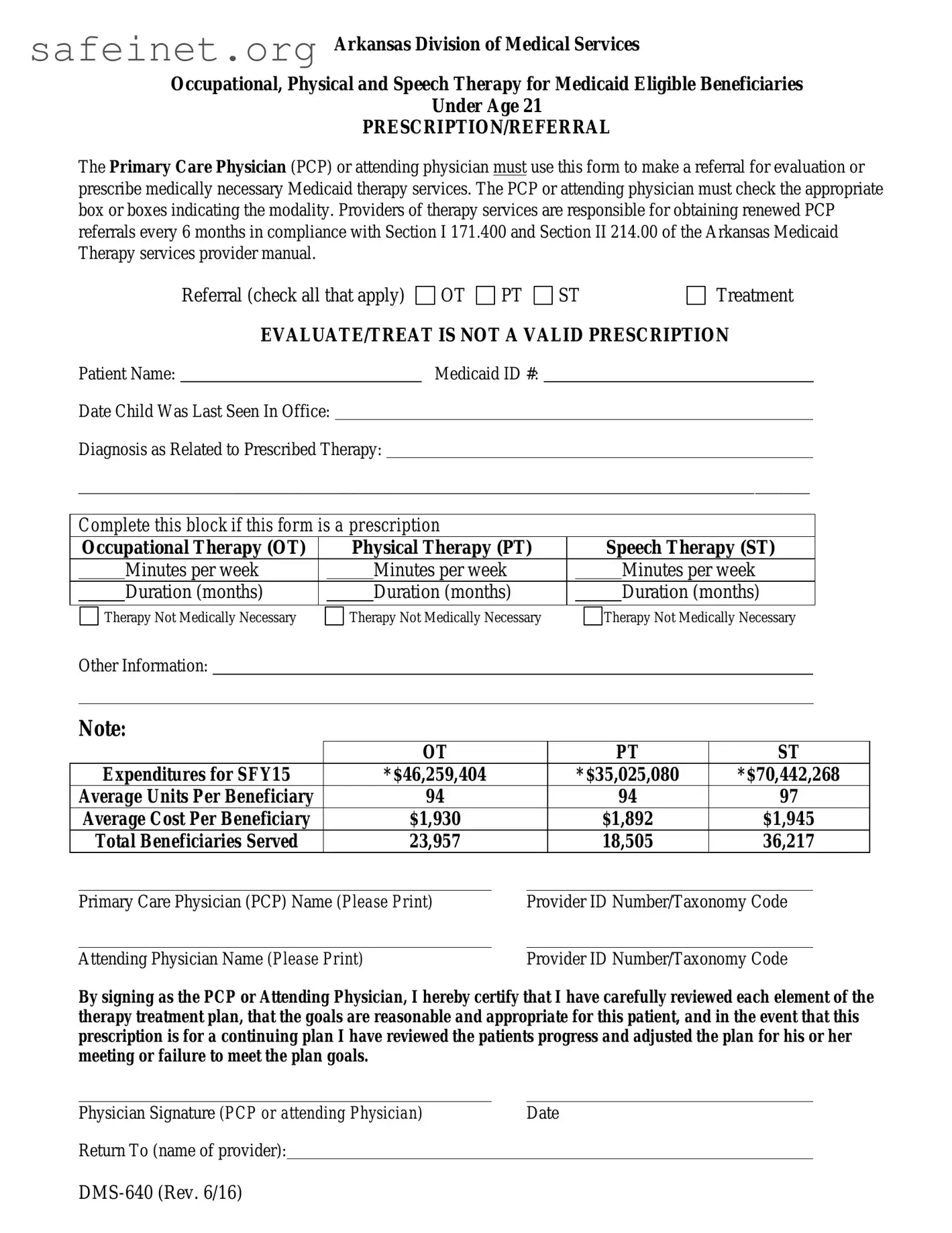
Arkansas Division of Medical Services
Occupational, Physical and Speech Therapy for Medicaid Eligible Beneficiaries
Under Age 21
PRESCRIPTION/REFERRAL
The Primary Care Physician (PCP) or attending physician must use this form to make a referral for evaluation or prescribe medically necessary Medicaid therapy services. The PCP or attending physician must check the appropriate box or boxes indicating the modality. Providers of therapy services are responsible for obtaining renewed PCP referrals every 6 months in compliance with Section I 171.400 and Section II 214.00 of the Arkansas Medicaid Therapy services provider manual.
EVALUATE/TREAT IS NOT A VALID PRESCRIPTION
Patient Name: |
|
Medicaid ID #: |
Date Child Was Last Seen In Office:
Diagnosis as Related to Prescribed Therapy:
______________________________________________________________________________________________
Complete this block if this form is a prescription
|
Occupational Therapy (OT) |
|
Physical Therapy (PT) |
|
Speech Therapy (ST) |
|
|
Minutes per week |
|
|
Minutes per week |
|
|
Minutes per week |
|
|
|
|
|
|
|
|
|
|
|
Duration (months) |
|
|
Duration (months) |
|
|
Duration (months) |
|
|
|
|
|
|
|
|
|
Therapy Not Medically Necessary
Therapy Not Medically Necessary
Therapy Not Medically Necessary
Other Information:
Note:
|
|
|
OT |
|
|
PT |
ST |
|
Expenditures for SFY15 |
|
*$46,259,404 |
|
|
*$35,025,080 |
*$70,442,268 |
|
Average Units Per Beneficiary |
|
94 |
|
|
94 |
97 |
|
|
Average Cost Per Beneficiary |
|
$1,930 |
|
|
$1,892 |
$1,945 |
|
Total Beneficiaries Served |
|
23,957 |
|
|
18,505 |
36,217 |
|
|
|
|
|
|
Primary Care Physician (PCP) Name (Please Print) |
|
Provider ID Number/Taxonomy Code |
|
|
|
|
|
|
|
Attending Physician Name (Please Print) |
|
|
Provider ID Number/Taxonomy Code |
By signing as the PCP or Attending Physician, I hereby certify that I have carefully reviewed each element of the therapy treatment plan, that the goals are reasonable and appropriate for this patient, and in the event that this prescription is for a continuing plan I have reviewed the patients progress and adjusted the plan for his or her meeting or failure to meet the plan goals.
Physician Signature (PCP or attending Physician) |
Date |
Return To (name of provider):
Instructions for Completion
Form DMS-640 – Occupational, Physical and Speech Therapy for Medicaid Eligible Beneficiaries Under Age 21 PRESCRIPTION/REFERRAL
If DMS-640 is used to make an initial referral for evaluation, check the box to indicate the appropriate therapy for the referral. After receiving the evaluation results and determining that therapy is necessary, you must use a separate DMS-640 form to prescribe the therapy. Check the treatment box for prescription and complete the form following the instructions below. If the referral and prescription are for previously prescribed services, you may check both boxes.
Patient Name – Enter the patient’s full name.
Medicaid ID # – Enter the patient’s Medicaid ID number.
Return To – To be completed by requesting provider to include therapy provider/address/fax/secure email.
Physician or Physician’s office staff must complete the following:
Date Child Was Last Seen In Office – Enter the date of the last time you saw this child. (This could be either for a complete physical examination, a routine check-up or an office visit for other reasons requiring your personal attention.)
Diagnosis as Related to Prescribed Therapy – Enter the diagnosis that indicates or establishes medical necessity for prescribed therapy.
Prescription block – If the form is used for a prescription, enter the prescribed number of minutes per week and the prescribed duration (in months) of therapy.
If therapy is not medically necessary at this time, check the box.
Other Information – Any other information pertinent to the child’s medical condition, plan of treatment, etc., may be entered.
Primary Care Physician (PCP) Name and Provider ID Number and/or Taxonomy Code – Print the name of the prescribing PCP and his or her provider identification number and/or taxonomy code.
Attending Physician Name and Provider ID Number and/or Taxonomy Code – If the Medicaid- eligible child is exempt from PCP requirements, print the name of the prescribing attending physician and his or her provider identification number and/or taxonomy code.
Physician Signature and Date – The prescribing physician must sign and date the prescription for therapy in his or her original signature.
Arkansas Medicaid’s criteria for electronic signatures as stated in Arkansas Code 25-31-103 must be met. For vendor’s EHR systems that are not configurable to meet the signature criteria, the provider should print, date and sign the DMS-640 form. Providers will be in compliance if a scanned copy of the original document is kept in a format that can be retrieved for a specific beneficiary. Most electronic health record systems allow this type of functionality.
When an electronic version of the DMS 640 becomes part of the physician/ or providers’ electronic health record, the inclusion of extraneous patient and clinic information does not alter the form.
*These therapy amounts include therapy provided in a Developmental Day Treatment Center (DDTCS)
The original of the completed form DMS-640 must be maintained in the child’s medical records by the prescribing physician. A copy of the completed form DMS-640 must be retained by the therapy provider.
 OT
OT 
 PT
PT  ST
ST