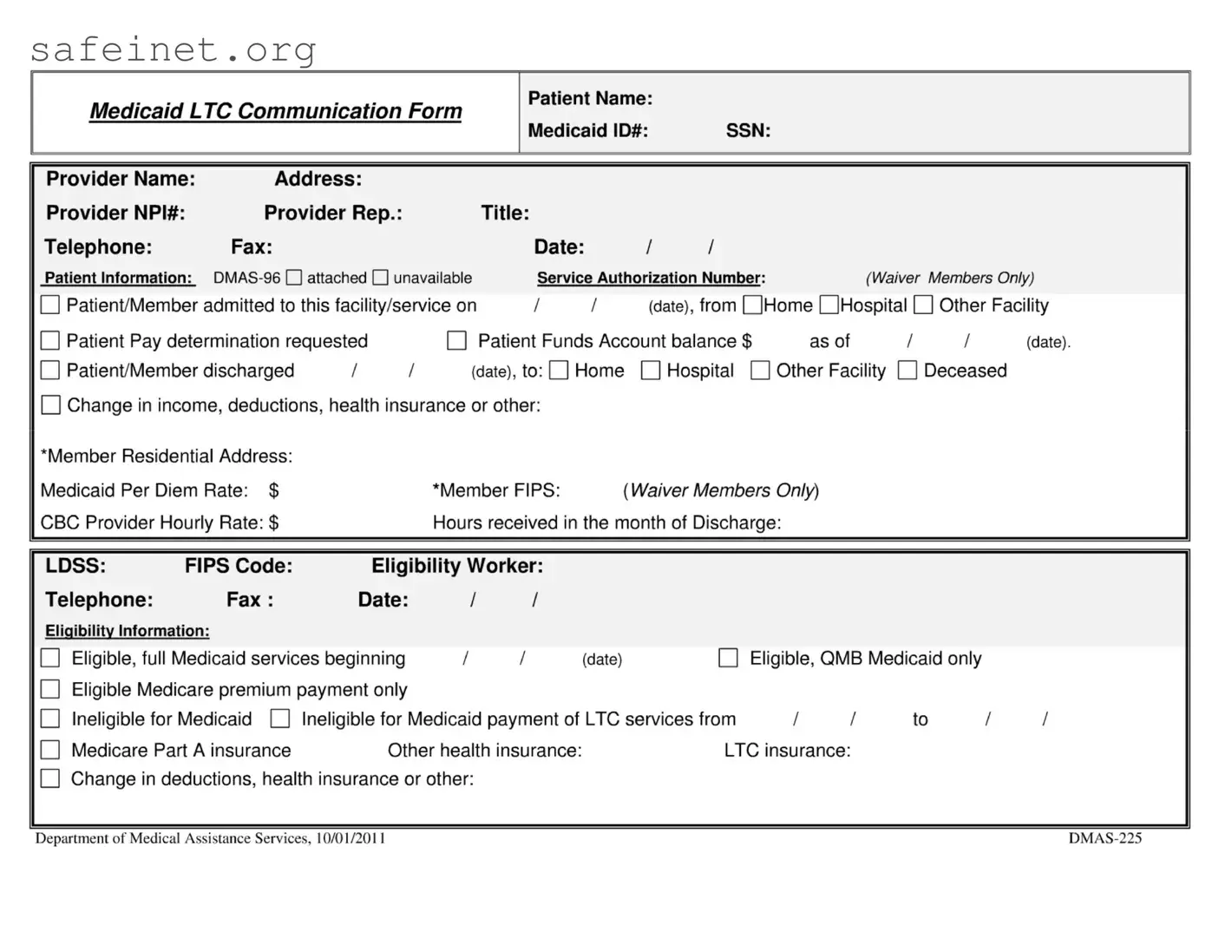
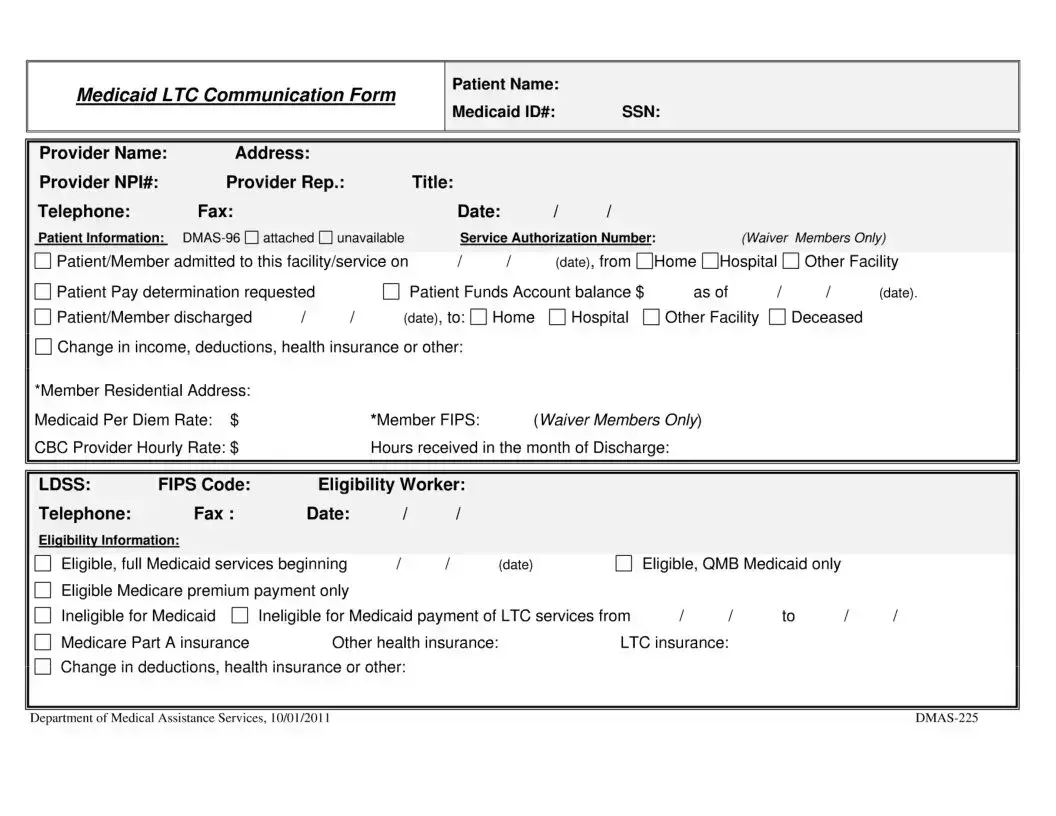
Medicaid LTC Communication Form
Provider Name: |
Address: |
|
|
|
|
|
|
|
|
|
|
Provider NPI#: |
Provider Rep.: |
|
|
Title: |
|
|
|
|
|
|
|
Telephone: |
Fax: |
|
|
|
Date: |
/ |
/ |
|
|
|
|
Patient Information: |
DMAS-96 attached unavailable |
|
Service Authorization Number: |
(Waiver Members Only) |
Patient/Member admitted to this facility/service on |
/ |
/ |
(date), from QHome OHospital |
|
Other Facility |
Patient Pay determination requested |
|
|
Patient Funds Account balance $ |
as of |
I |
I |
(date). |
Patient/Member discharged |
/ |
/ |
(date), to: |
Home |
|
Hospital О Other Facility |
|
Deceased |
|
Change in income, deductions, health insurance or other:
‘Member Residential Address:
Medicaid Per Diem Rate: $ |
‘Member FIPS: |
{WaiverMembers Only) |
CBC Provider Hourly Rate: $ |
Hours received in the month of Discharge: |
LDSS: FIPS Code: Eligibility Worker:
Telephone: |
Fax: |
Date: |
|
/ |
/ |
|
|
|
|
Eligibility Information: |
|
|
|
|
|
|
|
|
|
Eligible, full Medicaid services beginning |
1 |
/ |
(date) |
|
Eligible, QMB Medicaid only |
|
Eligible Medicare premium payment only |
|
|
|
|
|
|
|
Ineligible for Medicaid |
Ineligible for Medicaid payment of LTC services from |
II |
to |
II |
Medicare Part A insurance |
Other health insurance: |
LTC insurance: |
|
|
Change in deductions, health insurance or other:
Department of Medical Assistance Services, 10/01/2011 |
DMAS-225 |
Medicaid LTC Communication Form, Effective 10/01/2011 |
DMAS-225 |
PURPOSE OF FORM—To allow the local Department of Social Services (LDSS) and nursing facility (NF) or Community Based Care (CBC) Waiver Providers to exchange information regarding:
оThe Medicaid eligibility status of a patient/member;
оA change in the patient/member level of care;
оAdmission or discharge of a patient/member to an institution or Medicaid CBC services, or death of a patient;
оService Authorization Number for Medicaid CBC Services;
оOther information known to the provider that might cause a change in the eligibility status or patient pay amounts.
USE OF FORM—Initiated by either the LDSS or the provider of care. A new form must be prepared by the LDSS whenever there is any change in the member’s circumstances that results in a change in eligibility status or information needs to be given to the provider. The provider must use the form to document admission date, request Medicaid eligibility status, and notify the LDSS of changes in the patient’s circumstances, discharge or death.
NUMBER OF COPIES-Original and one copy for NF patients; original and two copies for CBC patients.
DISTRIBUTION OF COPIES—For NF patients/members, send the original to the nursing facility. For PACE patients/members, send the original to the PACE provider. For Medicaid CBC, send the original to the following individuals:
•Case Manager at DMAS for Tech Waiver, DMAS, Division of LTC, Waiver Unit, 600 E. Broad St., Richmond, VA 23219
•Case Manager at the Community Service Board for the MR and DS waivers Case Manager (Support Coordinator) for DD Waiver
•Service Facilitator for EDCD with consumer-directed service,
•Case Manager for any member with case management services, and
•Personal Care Provider for EDCD-personal care services and other services.
Place a copy of this form in the eligibility case file.
INSTRUCTIONS FOR PREPARATION OF THE FORM—Complete either the Provider or LDSS section as appropriate. At the top of the form, enter the Patient’s name, Social Security number and Medicaid identification number, if known.
Provider Section-Complete all data elements in the gray section. Check the appropriate boxes and complete all data elements as appropriate in the white section to the member’s circumstances. Providers should attach a copy of the DMAS-96 to this form when the patient is first admitted to care.
Waiver providers must advise the LDSS of the member residential address when different from the address from which this form originates and provide the Member FIPS code.
LDSS Section-Complete all data elements in the gray section. Check the appropriate boxes and complete all data elements in the white section as appropriate to the patient’s circumstances. Do not provide the source of an member’s income. If the member is ineligible for Medicaid payment of long-term care due to imposition of a penalty period, send a copy of this memo to the DMAS, Long-Term Care Division, 600 E. Broad St., Suite 1300, Richmond, Va. 23219