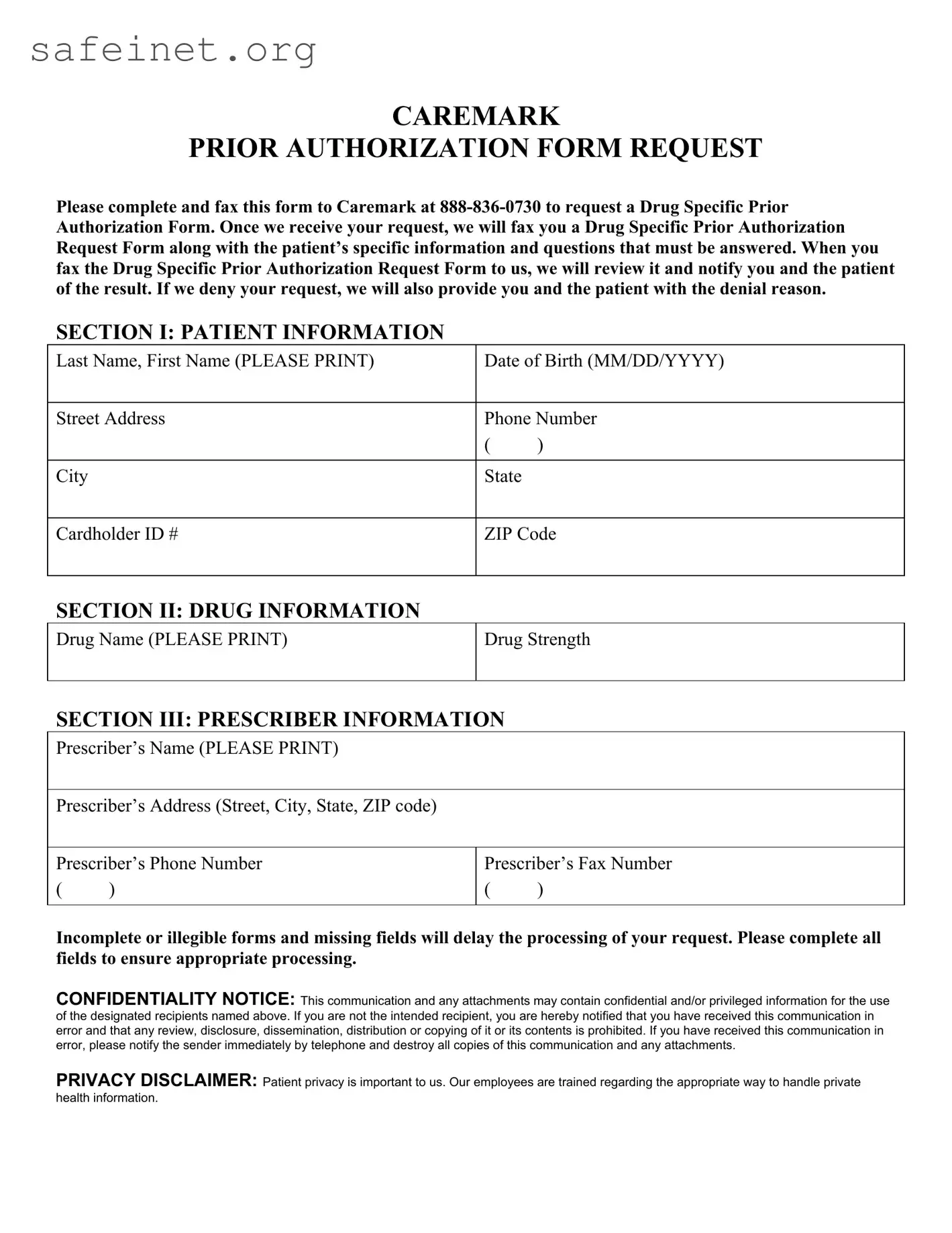
What is the CVS Prior Authorization Form?
The CVS Prior Authorization Form is a document required to request authorization for specific medications from Caremark. It is a crucial step in ensuring that prescribed drugs are covered by insurance before they can be dispensed. This form helps streamline the process and ensures that patients receive the medications they need in a timely manner.
How do I complete the form?
To complete the CVS Prior Authorization Form, carefully fill in all required fields. This includes patient information, drug details, and prescriber information. Make sure to print legibly to avoid processing delays. Incomplete or unclear submissions may cause significant setbacks in receiving authorization.
Where do I send the completed form?
After filling out the CVS Prior Authorization Form, fax it to Caremark at 888-836-0730. Ensure that you have completed all sections of the form, as this will facilitate a faster review and response from Caremark.
What happens after I submit the form?
Upon receiving your faxed request, Caremark will respond by sending a Drug Specific Prior Authorization Request Form. This will include the patient's specific information and any additional questions that must be answered to proceed with the authorization. It is essential to complete this form accurately and return it promptly.
How will I know the outcome of my request?
Once Caremark reviews the Drug Specific Prior Authorization Request Form you submitted, they will notify you and the patient of the decision. If the request is denied, Caremark will provide reasons for the denial, allowing prescribers to understand the next steps.
What should I do if my request is denied?
If your request for prior authorization is denied, review the denial reasons provided by Caremark. You may consider discussing alternatives with the prescribing doctor or re-evaluating the medication choice. In some cases, submitting additional information or modifications to the original request can lead to a successful outcome.
What if the form is incomplete or illegible?
Submitting an incomplete or illegible CVS Prior Authorization Form may lead to delays in processing your request. Ensure that all fields are accurately filled and written clearly. Double-check your submission before faxing it to avoid unnecessary complications.
What are the privacy considerations associated with this form?
Patient privacy is of utmost importance. The CVS Prior Authorization Form contains confidential information, and handling it appropriately is essential. Caremark employees are trained to manage private health information carefully, ensuring that only authorized individuals can access this data. If you receive the form in error, notify the sender immediately and destroy the document.
Can I get help if I have questions about filling out the form?
Yes, if you have questions or need assistance while completing the CVS Prior Authorization Form, it's advisable to contact Caremark directly. They can provide guidance and ensure that you understand all necessary sections for successful processing.