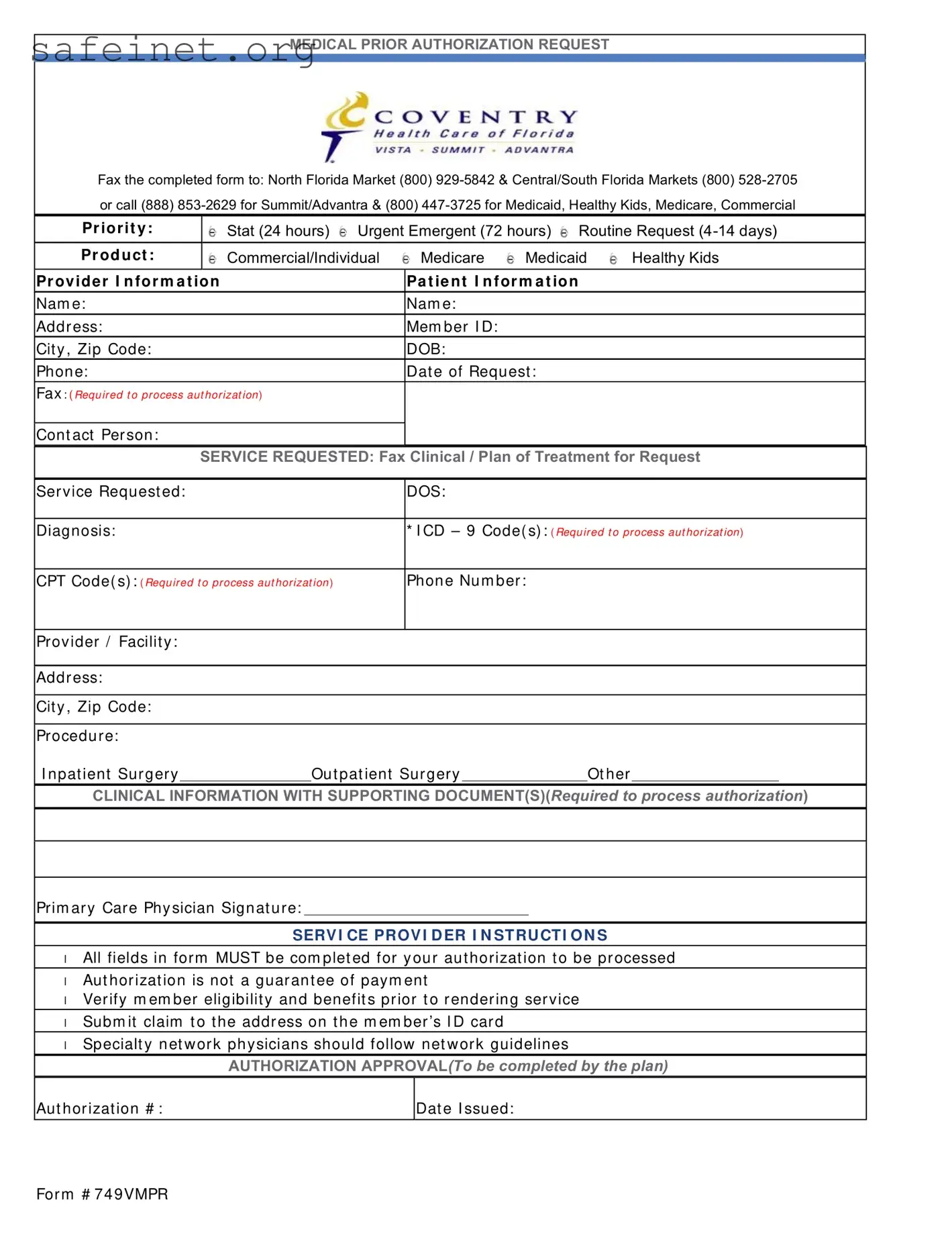
What is the Coventry Prior Authorization form?
The Coventry Prior Authorization form is a document that healthcare providers must complete to request approval for specific medical services, treatments, or procedures for their patients. This process ensures that the service is necessary and eligible for coverage under the patient's specific insurance plan.
How do I submit the Coventry Prior Authorization form?
To submit the completed form, fax it to the appropriate market. For the North Florida Market, use (800) 929-5842. For the Central/South Florida Markets, the fax number is (800) 528-2705. Alternatively, you can call (888) 853-2629 for Summit/Advantra or (800) 447-3725 for Medicaid, Healthy Kids, and Medicare inquiries.
What types of requests can be made using this form?
The form allows for several types of requests categorized by urgency: “Stat” for within 24 hours, “Urgent Emergent” for within 72 hours, and “Routine Request” for processing that takes 4 to 14 days. Services requested can include inpatient surgery, outpatient surgery, or other medical services.
What information is required on the form?
Essential details include the patient’s name, member ID, date of birth, and contact information. Additionally, the form requires information about the provider, the requested services, diagnosis codes (ICD-9), and procedure codes (CPT) to support the authorization request. All fields must be filled out for efficient processing.
Is prior authorization a guarantee of payment?
No, receiving prior authorization does not guarantee payment for the service. It simply indicates that the insurance company agrees that the service can be provided but does not confirm coverage. Providers are advised to verify the patient's eligibility and benefits before rendering the service.
Who can fill out the Coventry Prior Authorization form?
The form should be completed by a healthcare provider or their representative. This includes doctors, specialists, or administrative staff who have information regarding the patient's treatment and medical necessity for the requested service.
What should I do if I have questions about the form?
If you have questions or need assistance with the Coventry Prior Authorization form, you can contact Coventry customer service at the provided phone numbers. They can walk you through the process and clarify any uncertainties regarding the submission.
Where should I submit claims after receiving authorization?
After obtaining prior authorization, claims should be submitted to the address listed on the member’s ID card. This ensures that the claim is processed correctly and efficiently by the insurance provider.
What are the instructions for service providers?
All service providers must ensure that every field on the form is completed to avoid delays in authorization. Remember to follow any specific network guidelines, particularly for specialty network physicians. This can help in navigating the complexities of coverage more smoothly.