The Coventry Claim form shares similarities with the Appeal Request Form used in various health insurance contexts. Both documents allow individuals to request a review of a claim decision that they believe to be incorrect. They require essential information such as the member's details, the claim number, and an outline of the reasons for the appeal. Just like the Coventry form, the Appeal Request Form typically has a predefined submission timeframe, ensuring that disputes are handled promptly and efficiently. The goal is to help members recover costs they feel are unjustly denied.
Another document akin to the Coventry Claim form is the Medical Necessity Appeal Form. This form centers on ensuring that the requested medical services are deemed necessary and appropriate for the patient. The similarity lies in the structured process of challenging a denial based on medical necessity. Both forms require documentation and specifics surrounding the services rendered, supporting the claim that the care was needed. This helps facilitate a fair review, focusing on the quality of care received.
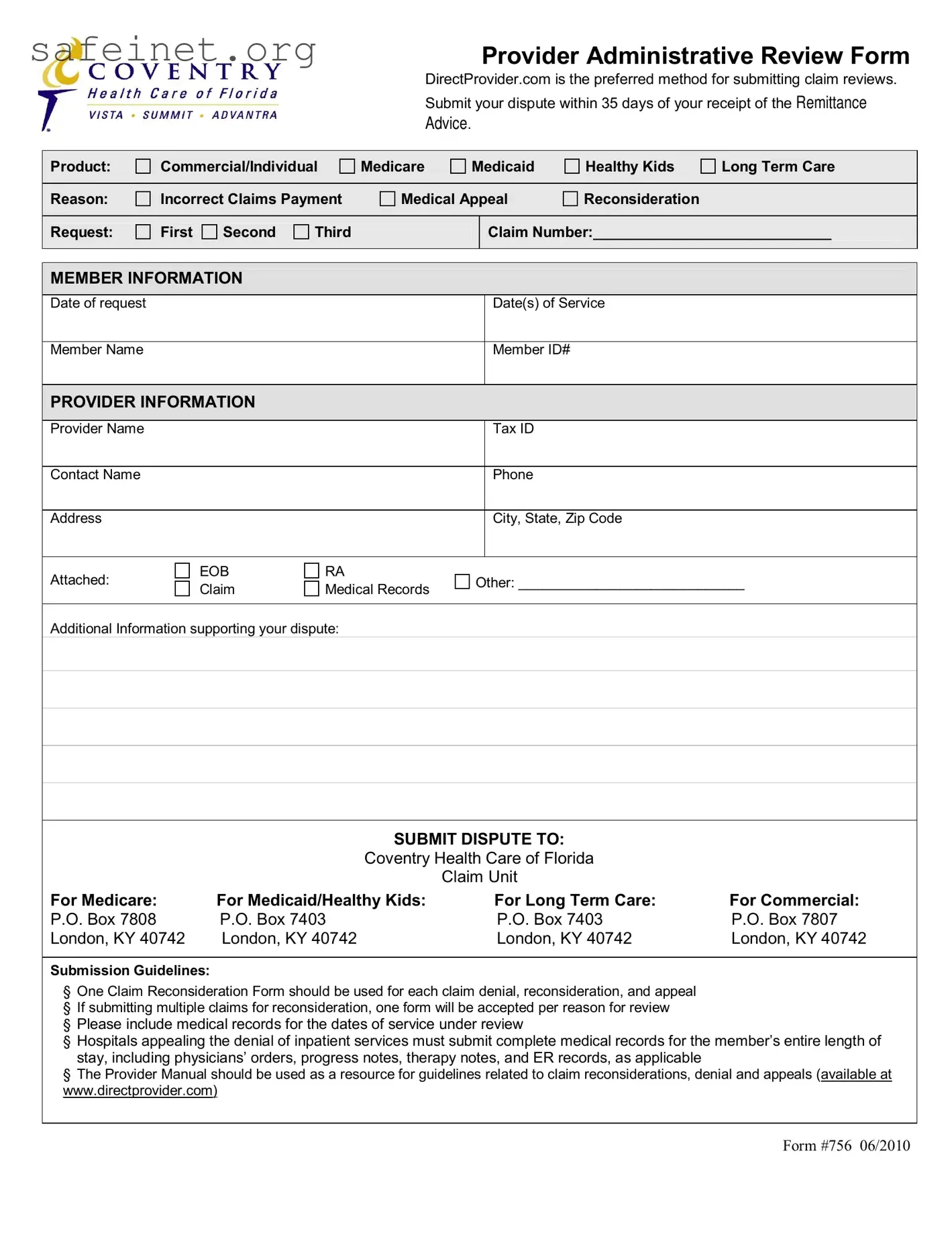
The Claim Reconsideration Form closely resembles the Coventry form as both pertain to challenging claims that have already been processed. They require detailed information similar to the claim submission process, offering clarity on the patient's identity and service details. These forms are designed to track the status of the claim through different stages of review and ensure that appropriate actions can be taken in light of new evidence or arguments presented.
The Patient Authorization Form also relates to the process initiated by the Coventry Claim form. This document grants consent for healthcare providers to share pertinent information regarding the individual’s claim. By facilitating open communication between patients and insurers, both forms ultimately aim to enhance transparency in the claims management process, helping claims reach a resolution more efficiently.
Similar to the Coventry Claim form is the Denial Letter. This document outlines why a claim was denied, including specific codes and reasons. While the Coventry form is a response to such denials, both documents play a part in the ongoing dialogue between patients and insurers. Each serves to clarify the intricacies of payment decisions and the rationale behind them, ensuring that all parties understand their positions.
An additional related document is the Provider Appeal Form. Like the Coventry Claim form, this form is used by healthcare providers to dispute payment reductions or denials. It captures vital details of the provider and the denied services, allowing them to articulate their position clearly. This emphasis on effective communication mirrors the principles behind the Coventry form, advocating for fair treatment in the claims process.
The Grievance Form stands in a similar capacity, representing concerns raised by members regarding their care or coverage decisions. This form prompts a review process akin to that of the Coventry Claim form by formally documenting issues that individuals face. Both forms seek redress for grievances, emphasizing procedural fairness in the healthcare system.
A notice of Claim Submission Guidelines can be viewed as closely aligned with the Coventry form as well. These guidelines direct individuals on the necessary steps to take when filing claims or appeals. They contain specifications and timelines just like the Coventry Claim form, reinforcing the importance of adhering to procedural rules to ensure successful resolution of disputes.
Additionally, the Authorization for Release of Information form bears resemblance to the Coventry Claim form. Both documents involve the dissemination of information critical to resolving claims disputes. By enabling providers to access necessary medical records for review, this form streamlines the claims reconsideration process, working in tandem with the Coventry form’s goals.
Finally, the Supplemental Claim Form serves a similar purpose to the Coventry Claim form. This document is used to provide additional evidence or documentation regarding a previous claim submission. Both forms are designed to clarify complicated issues surrounding claims, ensuring that all information is thoroughly considered during the reconsideration or appeals processes. Each aims to facilitate the protection of patient rights in securing fair reimbursement for healthcare services.