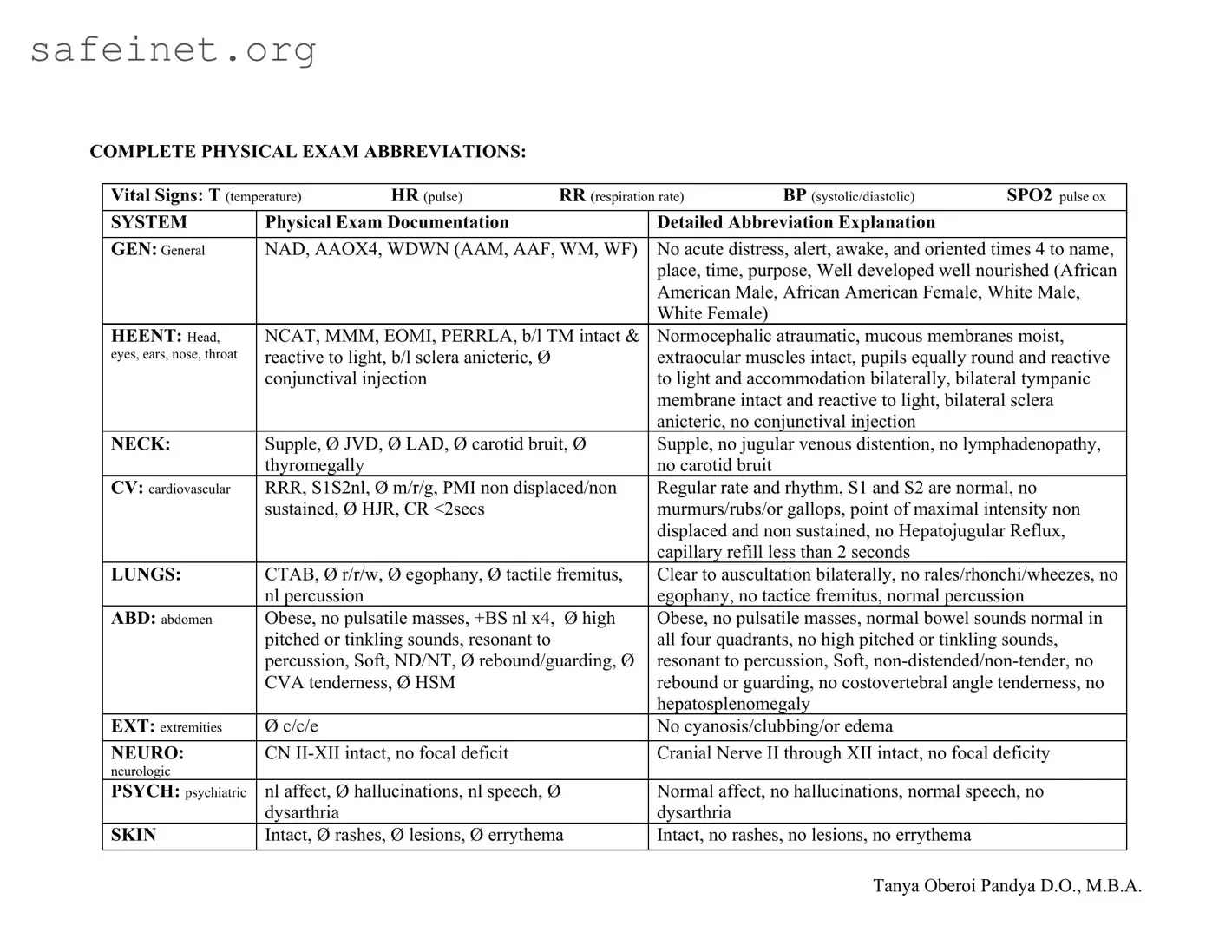
Vital Signs: T (temperature) |
HR (pulse) |
RR (respiration rate) |
BP (systolic/diastolic) |
SPO2 pulse ox |
|
|
|
|
|
SYSTEM |
Physical Exam Documentation |
|
Detailed Abbreviation Explanation |
|
|
|
|
GEN: General |
NAD, AAOX4, WDWN (AAM, AAF, WM, WF) |
No acute distress, alert, awake, and oriented times 4 to name, |
|
|
|
|
place, time, purpose, Well developed well nourished (African |
|
|
|
|
American Male, African American Female, White Male, |
|
|
|
|
White Female) |
|
|
HEENT: Head, |
NCAT, MMM, EOMI, PERRLA, b/l TM intact & |
Normocephalic atraumatic, mucous membranes moist, |
eyes, ears, nose, throat |
reactive to light, b/l sclera anicteric, Ø |
|
extraocular muscles intact, pupils equally round and reactive |
|
conjunctival injection |
|
to light and accommodation bilaterally, bilateral tympanic |
|
|
|
|
membrane intact and reactive to light, bilateral sclera |
|
|
|
|
anicteric, no conjunctival injection |
|
NECK: |
Supple, Ø JVD, Ø LAD, Ø carotid bruit, Ø |
Supple, no jugular venous distention, no lymphadenopathy, |
|
thyromegally |
|
|
no carotid bruit |
|
|
CV: cardiovascular |
RRR, S1S2nl, Ø m/r/g, PMI non displaced/non |
Regular rate and rhythm, S1 and S2 are normal, no |
|
sustained, Ø HJR, CR <2secs |
|
murmurs/rubs/or gallops, point of maximal intensity non |
|
|
|
|
displaced and non sustained, no Hepatojugular Reflux, |
|
|
|
|
capillary refill less than 2 seconds |
|
LUNGS: |
CTAB, Ø r/r/w, Ø egophany, Ø tactile fremitus, |
Clear to auscultation bilaterally, no rales/rhonchi/wheezes, no |
|
nl percussion |
|
|
egophany, no tactice fremitus, normal percussion |
ABD: abdomen |
Obese, no pulsatile masses, +BS nl x4, |
Ø high |
Obese, no pulsatile masses, normal bowel sounds normal in |
|
pitched or tinkling sounds, resonant to |
|
all four quadrants, no high pitched or tinkling sounds, |
|
percussion, Soft, ND/NT, Ø rebound/guarding, Ø |
resonant to percussion, Soft, non-distended/non-tender, no |
|
CVA tenderness, Ø HSM |
|
rebound or guarding, no costovertebral angle tenderness, no |
|
|
|
|
hepatosplenomegaly |
|
EXT: extremities |
Ø c/c/e |
|
|
No cyanosis/clubbing/or edema |
|
|
|
|
|
NEURO: |
CN II-XII intact, no focal deficit |
|
Cranial Nerve II through XII intact, no focal deficity |
neurologic |
|
|
|
|
|
|
PSYCH: psychiatric |
nl affect, Ø hallucinations, nl speech, Ø |
Normal affect, no hallucinations, normal speech, no |
|
dysarthria |
|
|
dysarthria |
|
|
SKIN |
Intact, Ø rashes, Ø lesions, Ø errythema |
Intact, no rashes, no lesions, no errythema |
|
|
|
|
|
|
|
|