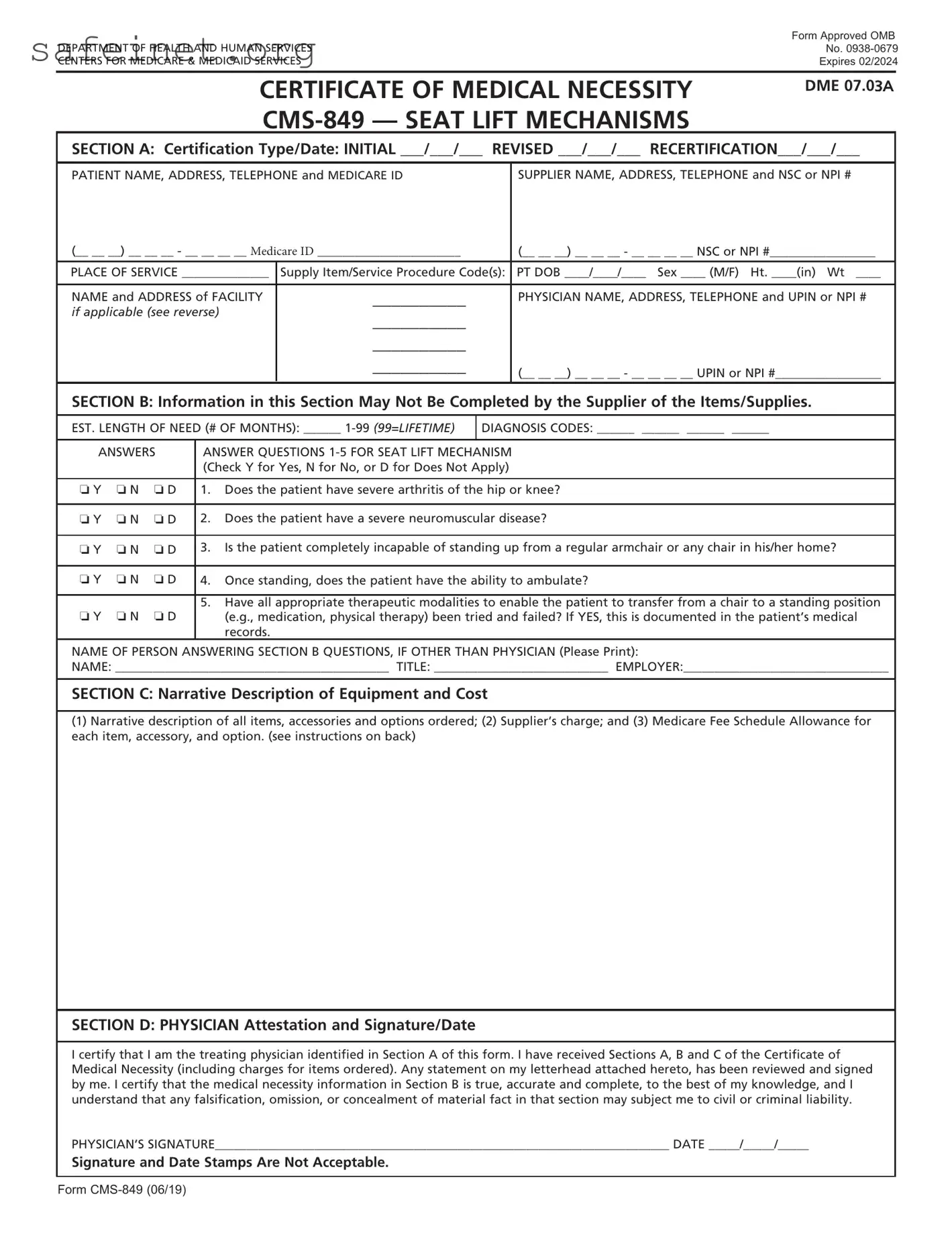
What is the purpose of the CMS 849 form?
The CMS 849 form, also known as the Certificate of Medical Necessity, is used to certify the medical necessity for seat lift mechanisms for patients. It ensures that Medicare covers the costs associated with this equipment, determining that the patient needs it for their care.
Who is responsible for completing the CMS 849 form?
The initial sections of the CMS 849 can be completed by the supplier or the physician. However, Section B, which gathers clinical information, must be completed by a qualified healthcare professional. A physician must review and sign the form to confirm the accuracy and validity of the information provided.
What information is required in Section A of the CMS 849?
Section A requires the patient’s personal information, including their name, address, telephone number, and Medicare ID. It also requests details about the supplier, including their name, address, and national supplier number, along with any relevant dates for initial certification or recertification.
What does Section B ask about the patient?
Section B contains questions about the patient’s medical condition that help establish the need for a seat lift. It inquires about the presence of severe arthritis, neuromuscular disease, the patient’s ability to stand from a chair, and whether previous therapeutic modalities have been attempted.
What details must be included in Section C?
In Section C, the supplier must provide a narrative description of all items ordered, including accessories and options. They must also include the supplier’s charge and the Medicare fee schedule allowance for each item, ensuring a clear understanding of costs associated with the equipment.
How does the physician confirm the information on the form?
The physician confirms the information by signing and dating Section D of the form. This signature certifies that they have reviewed all sections and that the medical necessity details in Section B are accurate and complete to the best of their knowledge.
What happens if the information submitted is inaccurate or incomplete?
If the information on the CMS 849 is found to be inaccurate or incomplete, it may result in delays in coverage or denial of claims for payment. The physician could also face civil or criminal liability for any falsifications or omissions.
How long does it take to complete the CMS 849 form?
On average, completing the CMS 849 form takes about 12 minutes. This includes time for reviewing instructions, gathering necessary data, and completing each section accurately.
Where can I find more information about filing claims associated with the CMS 849?
For detailed information on filing claims, it’s recommended to visit the official Medicare website at www.medicare.gov. This site offers resources and additional guidance for properly submitting claims.