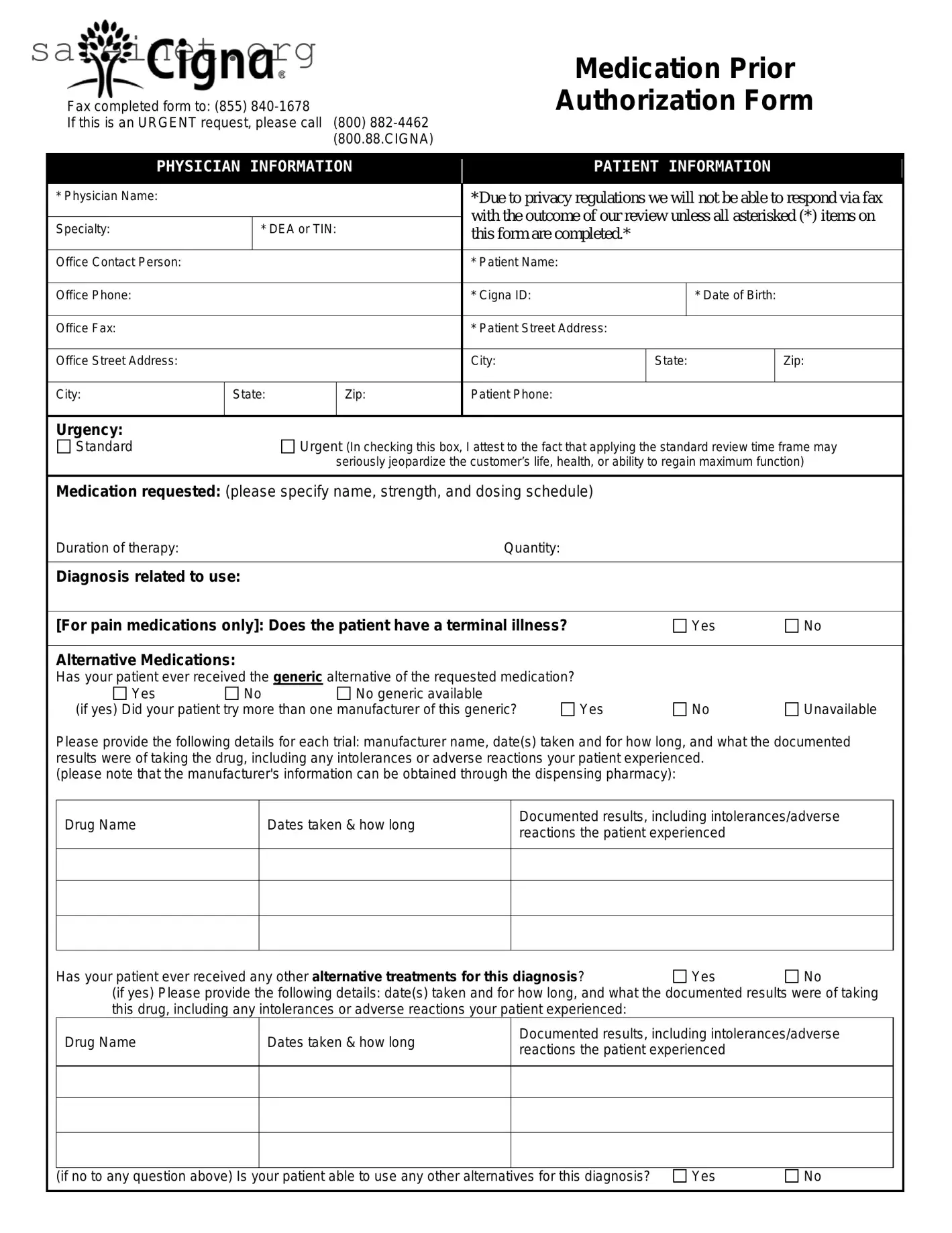
What is the purpose of the Cigna Prior Authorization form?
The Cigna Prior Authorization form is used to request prior approval for certain medications that Cigna may require before covering the cost. This process helps ensure that the medication is medically necessary for the patient’s condition.
How do I submit the Cigna Prior Authorization form?
You can submit the completed form by faxing it to (855) 840-1678. For urgent requests, it is recommended to call (800) 882-4462. Additionally, forms can be submitted online through CoverMyMeds or via SureScripts in your EHR, which may save time.
What information is required on the form?
Important details needed include the physician's name, patient’s Cigna ID, date of birth, and contact information. The form must also specify the requested medication, duration of therapy, and diagnosis related to the use of the medication. Ensure all required fields are filled out, as incomplete forms may delay processing.
What happens after I submit the form?
Once the form is submitted, Cigna will review the information provided. The standard response time for requests is typically 5 business days. If you submitted an urgent request, the review process may be expedited. However, outcomes will only be communicated via phone call if privacy regulations are met.
What should I do if the patient’s medication is not approved?
If a medication is not approved, you may receive a notice explaining the reason. In such cases, you might consider discussing alternative medications with the physician or reviewing other treatment options that could be more suitable for the patient’s needs.
Can I appeal the decision if the prior authorization is denied?
Yes. If the prior authorization request is denied, you can initiate an appeal. It is important to gather relevant documentation and communicate effectively with Cigna regarding the necessity of the medication for the patient’s health condition.
Is there a way to ensure faster processing of the prior authorization request?
For quicker processing, ensure that all mandatory fields on the form are completed accurately. Also, if the request is urgent due to serious health concerns, calling Cigna directly can expedite the review process. Utilizing online submission options may also enhance response times.