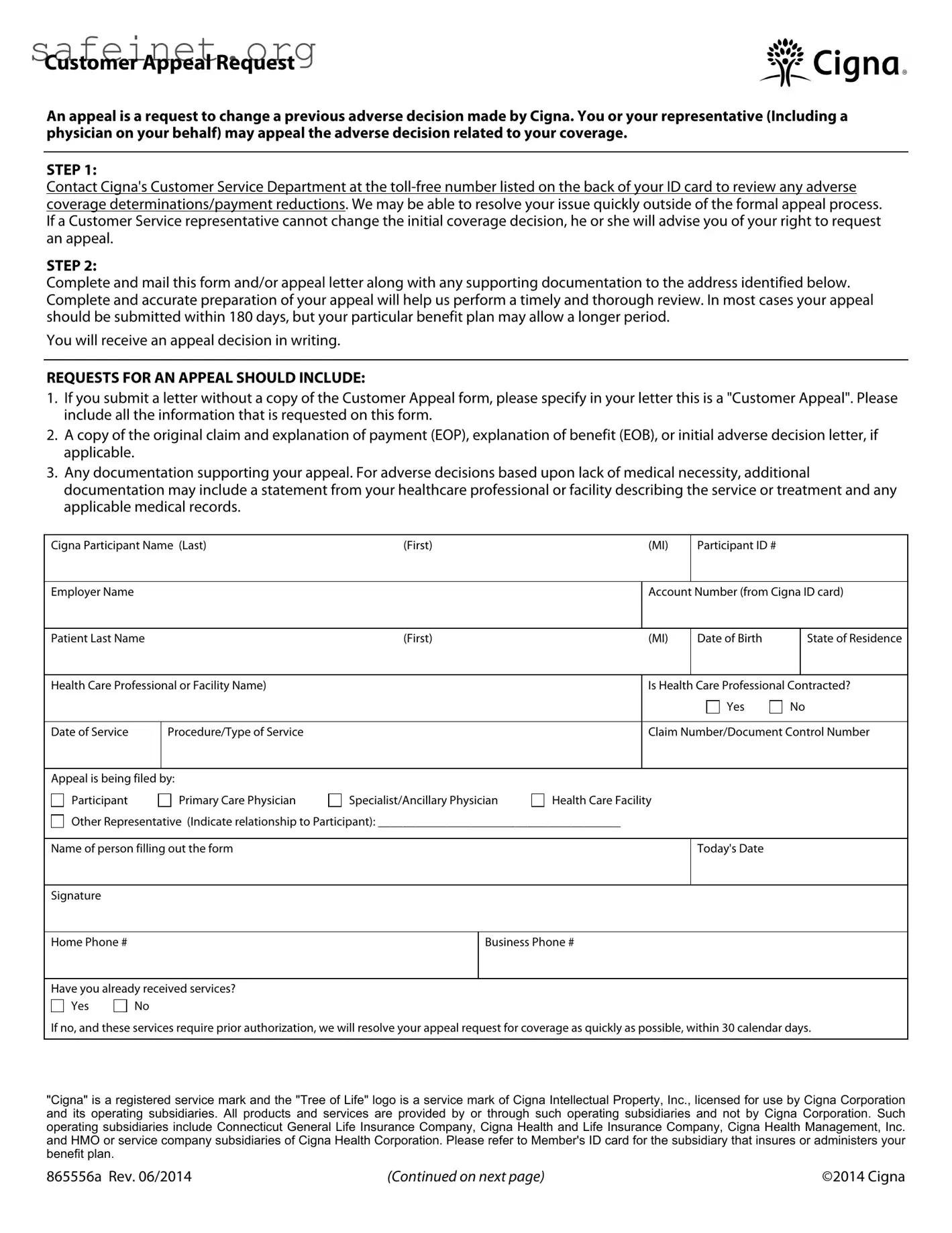
What is the purpose of the Cigna Appeal form?
The Cigna Appeal form serves as a formal request to change a previous adverse decision made by Cigna regarding coverage. Individuals, or their representatives such as physicians, can use this form to challenge decisions that affect their healthcare services or payment reductions.
How do I begin the appeal process?
To initiate the appeal, it is recommended to first contact Cigna's Customer Service Department. You can find a toll-free number on the back of your ID card. This step allows you to review the adverse coverage determinations directly. Sometimes, issues can be resolved quickly without going through the formal appeal process.
What information do I need to include when submitting the form?
Your appeal submission should include several key components. First, if you submit a letter instead of the form, confirm that it is a "Customer Appeal" and provide all requested information from the form. Additionally, include a copy of the original claim and any relevant letters regarding adverse decisions, as well as supporting documentation related to your appeal.
How long do I have to submit my appeal?
Typically, you should submit your appeal within 180 days of the adverse decision. However, some benefit plans might allow for a longer submission period. Always check the specific terms of your plan to ensure compliance.
What happens after I submit my appeal?
Once your appeal is submitted, Cigna will review your case and respond in writing. You will receive a formal decision regarding the appeal, which should clarify whether the initial decision has been overturned or upheld.
Is there a specific address to send my appeal request?
The address for submitting your appeal request depends on your ID card. If it indicates "Cigna Network," use the following address: Cigna Appeals Unit, P.O. Box 188011, Chattanooga, TN 37422-8011. For "GW - Cigna Network," send it to P.O. Box 188062, Chattanooga, TN 37422-8062. Ensure you only send appeal requests to avoid delays.
What types of issues can I appeal?
Common reasons for appeals include requests for in-network coverage, coverage exclusions, and denials based on medical necessity. You can also appeal decisions regarding payment reductions or requests related to previously denied claims. Specify the reason for your appeal clearly in your submission.
Can I get help with my appeal?
Yes, you may have a representative, such as your physician, assist you in the appeal process. When appointing a representative, make sure to indicate their relationship to you on the form and provide their contact information. This can help facilitate communication between Cigna and your representative.
What should I do if my appeal is denied?
If your appeal is denied, you may have options for a second appeal or a request for an external review, depending on the provisions of your plan. These steps should be outlined in the initial response Cigna provides. Understanding your rights concerning further appeals is crucial to ensure you have exhausted all available options.

 Request for
Request for 
 Coverage Exclusion or Limitation
Coverage Exclusion or Limitation
 Maximum Reimbursable Amount
Maximum Reimbursable Amount
 Inpatient Facility Denial (Level of Care, Length of Stay)
Inpatient Facility Denial (Level of Care, Length of Stay)
 Mutually Exclusive, Incidental procedure code denials
Mutually Exclusive, Incidental procedure code denials
 Additional reimbursement to your out of network health care professional for a procedure code modifier
Additional reimbursement to your out of network health care professional for a procedure code modifier
 Experimental/Investigational Procedure
Experimental/Investigational Procedure
 Medical Necessity
Medical Necessity
 Timely Claim Filing (without proof)
Timely Claim Filing (without proof)
 Benefits reduced due to
Benefits reduced due to