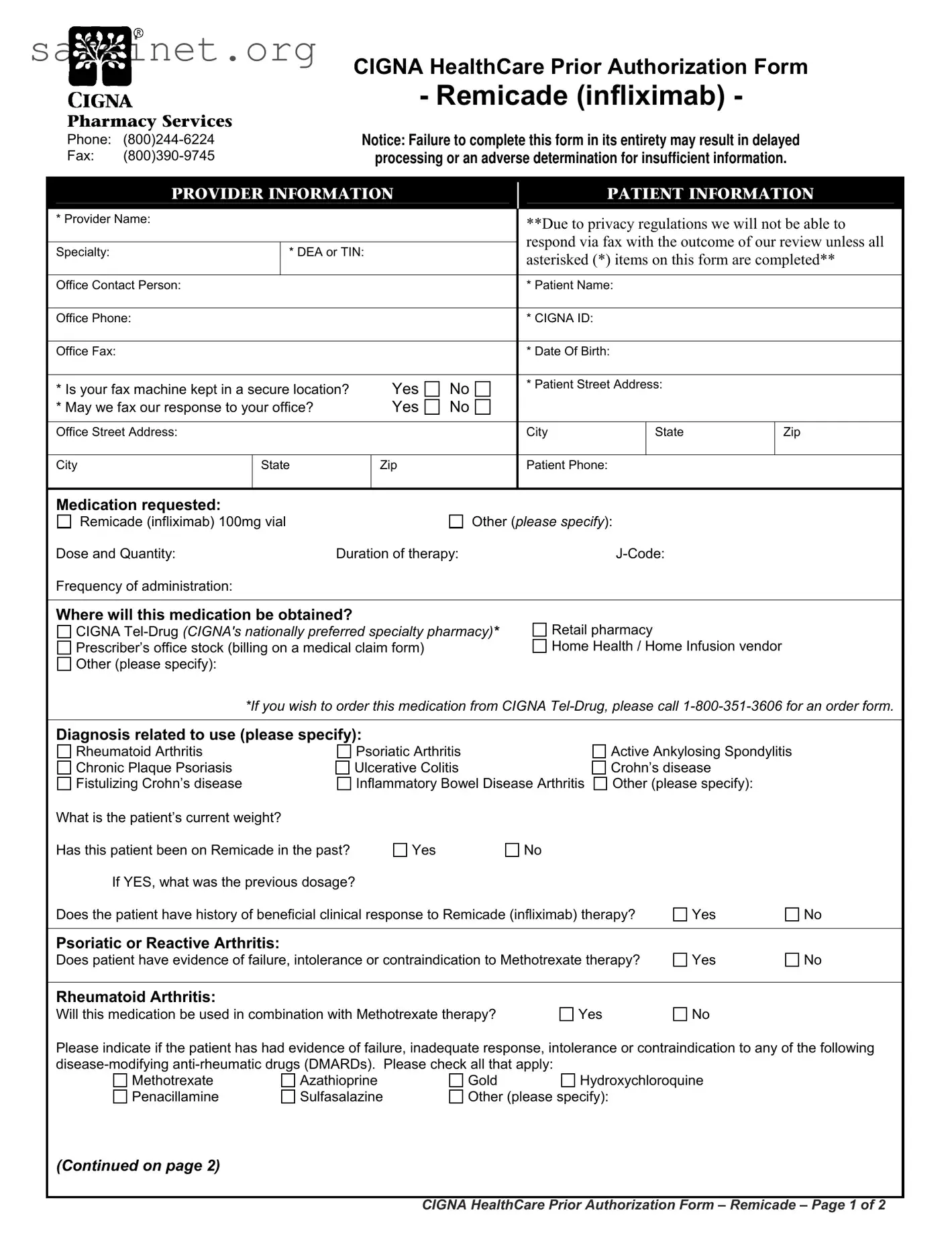
Pharmacy Services
Phone: (800)244-6224
Fax: (800)390-9745
CIGNA HealthCare Prior Authorization Form
- Remicade (infliximab) -
Notice: Failure to complete this form in its entirety may result in delayed
processing or an adverse determination for insufficient information.
|
|
PROVIDER INFORMATION |
|
|
PATIENT INFORMATION |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
* Provider Name: |
|
|
|
|
**Due to privacy regulations we will not be able to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
respond via fax with the outcome of our review unless all |
|
|
|
Specialty: |
|
* DEA or TIN: |
|
|
|
|
|
|
|
|
asterisked (*) items on this form are completed** |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office Contact Person: |
|
|
|
|
* Patient Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office Phone: |
|
|
|
|
* CIGNA ID: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office Fax: |
|
|
|
|
* Date Of Birth: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
* Is your fax machine kept in a secure location? |
Yes |
No |
* Patient Street Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
* May we fax our response to your office? |
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office Street Address: |
|
|
|
|
City |
State |
Zip |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City |
State |
Zip |
|
Patient Phone: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medication requested:
Remicade (infliximab) 100mg vial |
|
Other (please specify): |
|
|
|
Dose and Quantity: |
Duration of therapy: |
|
J-Code: |
|
|
|
Frequency of administration: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Where will this medication be obtained? |
|
|
|
|
|
|
CIGNA Tel-Drug (CIGNA's nationally preferred specialty pharmacy)* |
Retail pharmacy |
|
|
|
Prescriber’s office stock (billing on a medical claim form) |
Home Health / Home Infusion vendor |
|
|
Other (please specify): |
|
|
|
|
|
|
|
*If you wish to order this medication from CIGNA Tel-Drug, please call 1-800-351-3606 for an order form. |
|
|
|
|
|
|
Diagnosis related to use (please specify): |
|
|
|
|
|
Rheumatoid Arthritis |
|
Psoriatic Arthritis |
|
Active Ankylosing Spondylitis |
|
|
Chronic Plaque Psoriasis |
|
Ulcerative Colitis |
|
Crohn’s disease |
|
|
Fistulizing Crohn’s disease |
|
Inflammatory Bowel Disease Arthritis |
Other (please specify): |
|
|
What is the patient’s current weight? |
|
|
|
|
|
|
|
Has this patient been on Remicade in the past? |
Yes |
No |
|
|
|
|
If YES, what was the previous dosage? |
|
|
|
|
|
Does the patient have history of beneficial clinical response to Remicade (infliximab) therapy? |
Yes |
No |
|
|
|
|
|
|
|
|
Psoriatic or Reactive Arthritis: |
|
|
|
|
|
|
|
Does patient have evidence of failure, intolerance or contraindication to Methotrexate therapy? |
Yes |
No |
|
|
|
|
|
|
|
|
Rheumatoid Arthritis: |
|
|
|
|
|
|
|
Will this medication be used in combination with Methotrexate therapy? |
Yes |
|
No |
|
|
Please indicate if the patient has had evidence of failure, inadequate response, intolerance or contraindication to any of the following
disease-modifying anti-rheumatic drugs (DMARDs). Please check all that apply: |
|
Methotrexate |
Azathioprine |
Gold |
Hydroxychloroquine |
Penacillamine |
Sulfasalazine |
Other (please specify): |
(Continued on page 2)
CIGNA HealthCare Prior Authorization Form – Remicade – Page 1 of 2
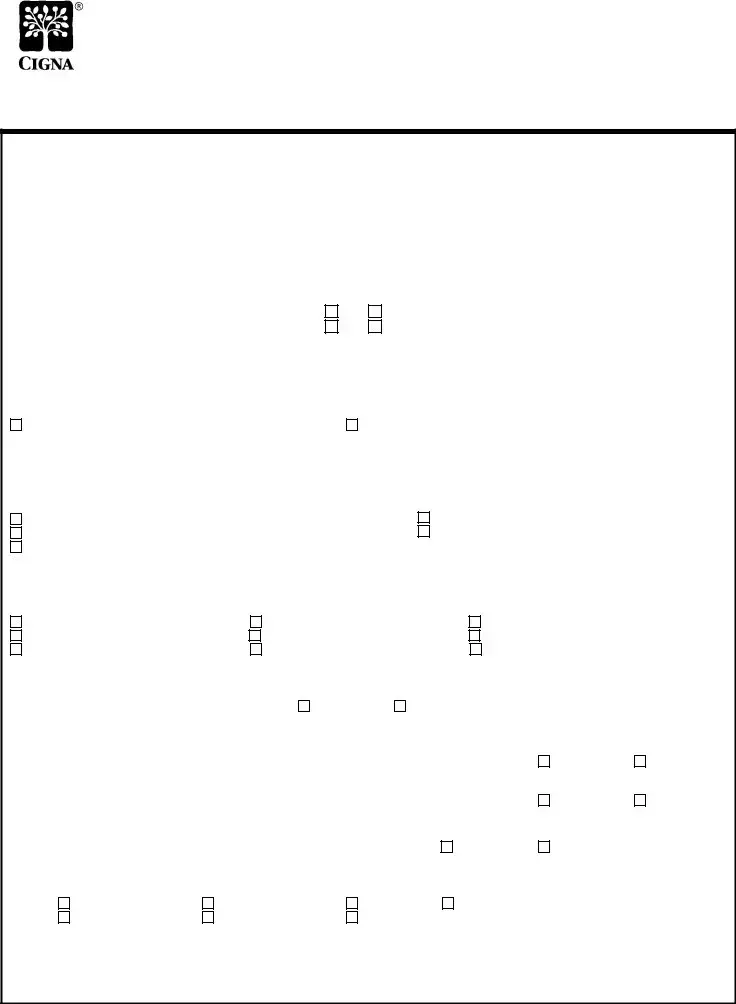
If YES, please specify which medications:
Which of the following methods was used to measure the patient’s disease progression PRIOR to therapy on Remicade? (Check all that apply):
Health Assessment Questionnaire Disease Index (HAQ-DI) |
Visual Analogue scale (VAS) |
Likert scales of global response to pain by the patient/doctor |
Global Arthritis Score (GAS) |
Clinical Disease Activity Index (CDAI) |
Simplified Disease Activity Index (SDAI) |
Progression of radiographic damage of involved joints |
Disease Activity Scale (DAS) score |
Disease Activity Score based on 28-joint evaluation (DAS28) score Disease Activity Scale (DAS) score
Elevation of ESR (> 28 mm/hr), or C-reactive protein (CRP) (2x the upper limit of normal)
Other (please specify) :
If this is a request for CONTINUED THERAPY (after at least 16 weeks of treatment), has the patient shown beneficial response to treatment with Remicade based on any of the following measurements? (Check all that showed a beneficial response to Remicade therapy):
Health Assessment Questionnaire Disease Index (HAQ-DI) |
Visual Analogue scale (VAS) |
Likert scales of global response to pain by the patient/doctor |
Global Arthritis Score (GAS) |
Clinical Disease Activity Index (CDAI) |
Simplified Disease Activity Index (SDAI) |
Disease Activity Scale (DAS) score |
ESR or C-reactive protein (CRP) |
Disease Activity Score based on 28-joint evaluation (DAS28) score Disease Activity Scale (DAS) score
At least a 20% improvement according to ACR 20% response criteria
Other (please specify) :
Chronic Plaque Psoriasis:
Does the patient have history of beneficial clinical response to Remicade (infliximab) therapy?
Is the patient a candidate for systemic therapy?
Is the severity great enough that the patient is a candidate for Photo Therapy?
Is this a request for a renewal of a previously granted authorization?
If YES, please document improvement since beginning therapy:
Crohn’s Disease:
Has the patient had failure, contraindication, or intolerance to conventional therapies such as aminosalicylate, corticosteroids, or immunomodulators?
Yes 
 No
No
Did the patient have a failure or intolerance to adalimumab (Humira) therapy?
Fistulizing Crohn’s Disease:
How long have fistulas persisted?
Inflammatory Bowel Disease Arthritis:
Has the patient had failure, contraindication, or intolerance to sulfasalazine, azathioprine, steroids, or, methotrexate?
Ankylosing Spondylitis:
Has the patient had failure, contraindication, or intolerance to non-steroidal anti-inflammatory drugs (NSAIDs)?
Ulcerative colitis:
Has the patient had failure, contraindication, or intolerance to conventional therapies such as corticosteroids (e.g, prednisone, methylprednisolone), 5-aminosalicylic acid agents (e.g., sulfasalazine, mesalamine, balsalazide), or immunosuppressants (e.g., azathioprine, cyclosporine, 6-mercaptopurine)?
Yes |
No |
If YES, please specify which medications: |
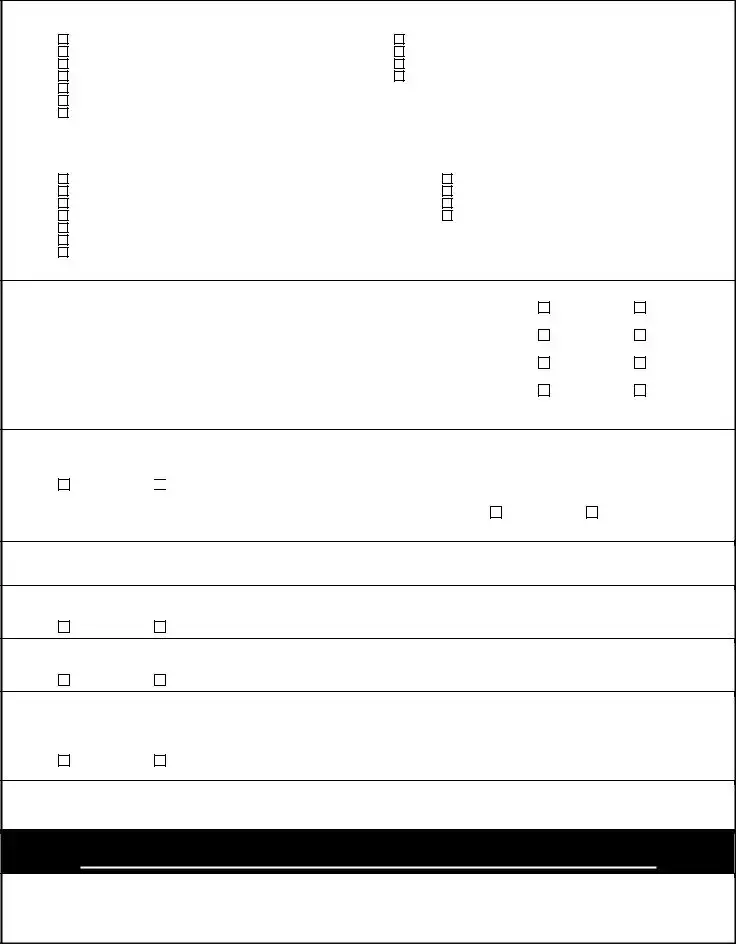
Additional pertinent information:
CIGNA HealthCare’s coverage position on this and other medications may be viewed online at:
http://www.cigna.com/customer_care/healthcare_professional/coverage_positions
Please fax completed form to (800)390-9745.
Our standard response time for prescription drug coverage requests is 2-4 business days. If your request is urgent, it is important that you call Pharmacy Services to expedite the request. View our formulary on line at http://www.cigna.com.
“CIGNA Pharmacy Management” or “CIGNA HealthCare” refer to various operating subsidiaries of CIGNA Corporation. Products and services |
V 041610 |
|
are provided by these subsidiaries and not by CIGNA Corporation. These subsidiaries include Connecticut General Life Insurance Company, Tel- |
|
Drug, Inc., Tel-Drug of Pennsylvania, L.L.C., and HMO or service company subsidiaries of CIGNA Health Corporation. |
|
CIGNA HealthCare Prior Authorization Form - Remicade - Page 2 of 2

 No
No