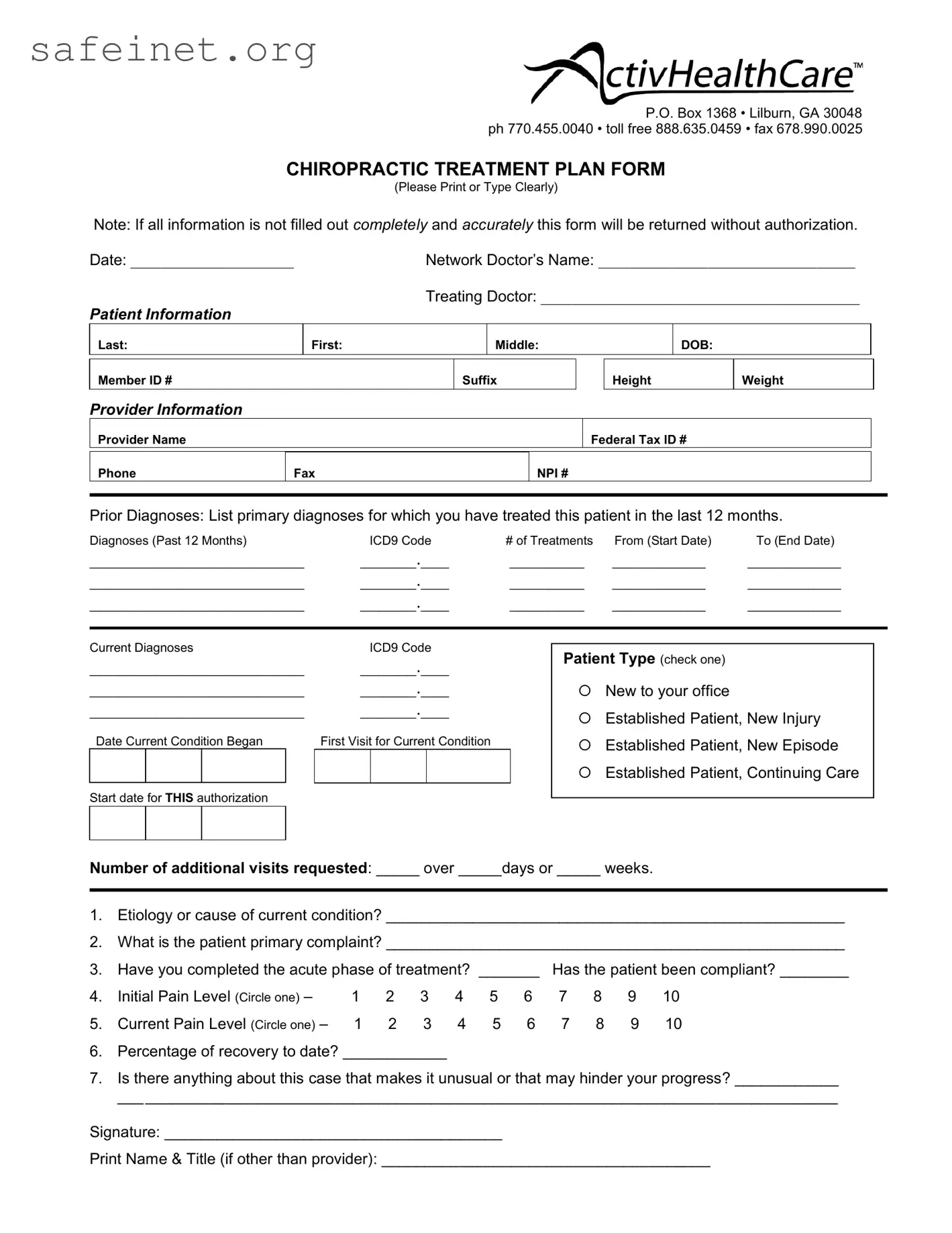
What is the purpose of the Chiropractic Treatment Plan form?
This form serves as a vital tool for documenting patient information and treatment details. It ensures that all necessary data is collected for authorization purposes, allowing healthcare providers to outline the course of treatment effectively. Accurate and complete information helps in both managing patient care and facilitating insurance claims.
What information do I need to provide about myself?
Patients must provide several key details. This includes your last name, first name, middle initial, date of birth, and member ID. Additionally, it's important to include your height and weight. Providing accurate personal information is essential for establishing a clear treatment plan tailored to your needs.
Who should fill out the provider information section?
The healthcare provider responsible for your treatment should complete the provider information section. This includes writing the name of the provider, their federal tax ID number, and contact details. Ensuring this section is filled out correctly aids in identifying the submitting provider for any future correspondence or clarifications.
What are prior diagnoses, and why do they matter?
Prior diagnoses refer to the primary conditions for which the patient received treatment in the past year. Listing this information is crucial, as it helps the current provider understand your medical history and make informed decisions about ongoing treatment plans. Accurate documentation of past diagnoses also supports insurance claims and necessitates better continuity of care.
What does the section on current diagnoses require?
The current diagnoses section requires providers to specify any diagnoses relevant to your present condition. Each diagnosis must be linked to an ICD9 code, providing a standardized way of identifying the condition. This information is essential for both clinical assessment and insurance purposes.
What is the significance of the patient type options?
Defining your patient type is important for the treatment provider. It indicates whether you are new to the office, an established patient with a new injury, or continuing care for a prior condition. This classification influences the treatment strategy and the number of visits authorized for submittal.
Why do I need to indicate the number of additional visits requested?
Indicating the number of additional visits needed and the timeframe for those visits is crucial for obtaining authorization from insurance. It allows the provider to justify ongoing treatment and helps manage your care plan effectively. Without this information, the form may be returned for further clarification.
What do the pain level options mean?
Patients are asked to rate their initial and current pain levels on a scale of 1 to 10. This subjective measure helps healthcare providers gauge the severity of your condition and assess progress throughout treatment. Tracking changes in pain levels can inform necessary adjustments to your therapy.
What should I discuss if there is something unusual about my case?
If you have any concerns that might affect your treatment progress, it is essential to communicate these clearly in the provided section. This could include underlying health issues, specific challenges in recovery, or unique medical concerns. Sharing this information allows the provider to better tailor the treatment plan to suit your individual circumstances.
What should I do after completing the Chiropractic Treatment Plan form?
Once the form is complete, it needs to be signed by the treating doctor or authorized representative. Ensure all fields are filled out accurately before submission. Incomplete forms may be returned for clarification, causing delays in the authorization process. Keep a copy of the completed form for your records as well.