|
|
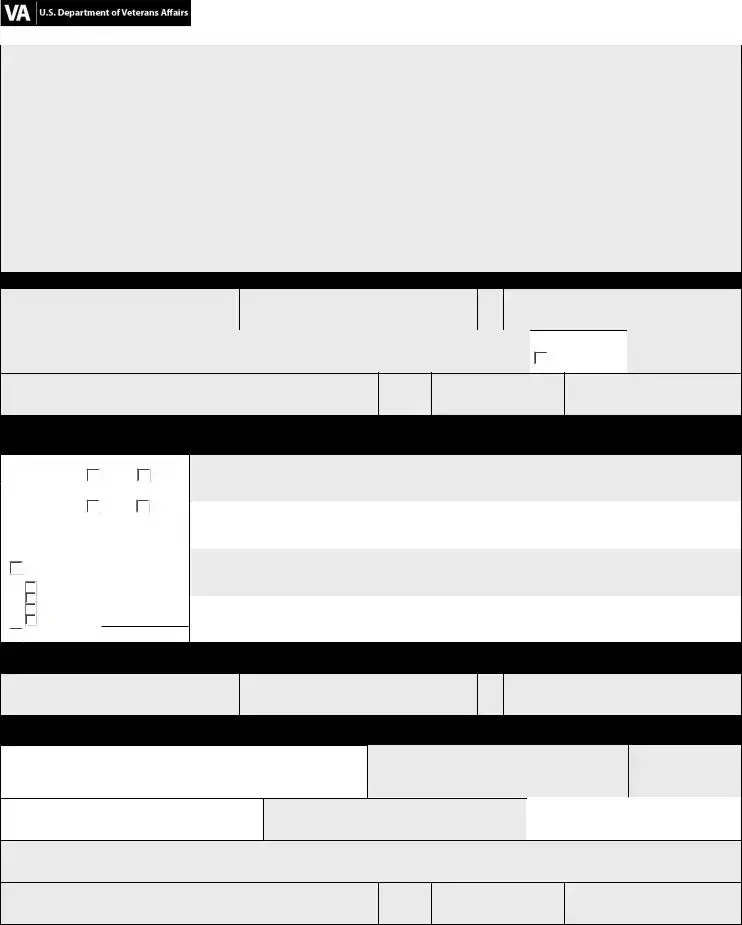
OMB Number: 2900-0219 Est. Burden: 10 minutes |
|
|
|
|
|
CHAMPVA Claim Form |
VA Health Administration Center |
CHAMPVA PO Box 469064 Denver CO 80246-9064 1-800-733-8387 |
Attention: After reviewing the following information, complete the form in its entirety (print or type only) and return with the required documentation.
Claim form usage: This form is to be completed by the patient, sponsor, or guardian and is mandatory for all beneficiary claims. This claim form is NOT to be used for provider submitted claims.
Other health insurance (OHI): If OHI exists, attach OHI’s Explanation of Benefits (EOB) to the provider’s itemized billing statement(s). Dates of service and provider charges on EOB must match billing statements.
Timely filing requirement: Claims must be received no later than one year after the date of service or, in the case of inpatient care, within one year of the discharge date.
Itemized billing statements: An itemized statement must be attached and contain:
•patient name, date of birth, and CHAMPVA Identification Card (ID-Card) Member Number (same as patient’s Social Security number);
•provider name, degree, tax identification number (TIN), address and telephone number; and
•service dates, itemized charges and appropriate procedure/diagnosis codes for each service (i.e. CPT-4, HCPCS, and ICD-9-CM codes), including narrative descriptions. Pharmacy claims are to include name, quantity, strength, and NDC of each drug.
Section I - Patient Information
Last Name (this is a mandatory field)
First Name (this is a mandatory field)
CHAMPVA Member Number (this is a mandatory field)
Street Address |
|
Date of Birth (mm/dd/yyyy) |
 Check if new
Check if new
Telephone Number (include area code)
Section II - Other Health Insurance (OHI) Information
By law, other coverage must be reported. Except for CHAMPVA supplemental policies, CHAMPVA is always the secondary payer.
If more space is needed, please continue in the same format on a separate sheet.
• Was treatment for a work-related injury or
•Was treatment for an injury or accident outside of work?
•Is patient covered by other primary health insurance to include coverage through a family member (supplemental or secondary insurance excluded)?
Yes (check type below and provide coverage information on the right)
 employer sponsored (group) private (non group)
employer sponsored (group) private (non group)
 Medicare (Part A or B) other (specify)
Medicare (Part A or B) other (specify)

 no (proceed to Section III)
no (proceed to Section III)
Name of Other Health Insurance (OHI)
|
|
OHI Policy Number |
OHI Telephone Number (include area code) |
|
|
|
|
Name of Other Health Insurance (OHI)
OHI Policy Number |
OHI Telephone Number (include area code) |
|
|
Section III - Sponsor Information
CHAMPVA Member Number (this is a mandatory field)
Section IV - Claimant Certification
Federal Laws (18 USC 287 and 1001) provide for criminal penalties for knowingly submitting or making false, fictitious, or fraudulent statements or claims.
I certify that the above information and attachments are correct and represent actual services, dates, and fees charged. (Sign and
4date on right.) If certification is signed by a person other than the
patient, complete the information the signature and date.
Signature (type if electronic)
|
MI |
Relationship to Patient |
|
|
|
Telephone Number (include area code)
VA FORM |
10-7959a |
MAY 2010 |
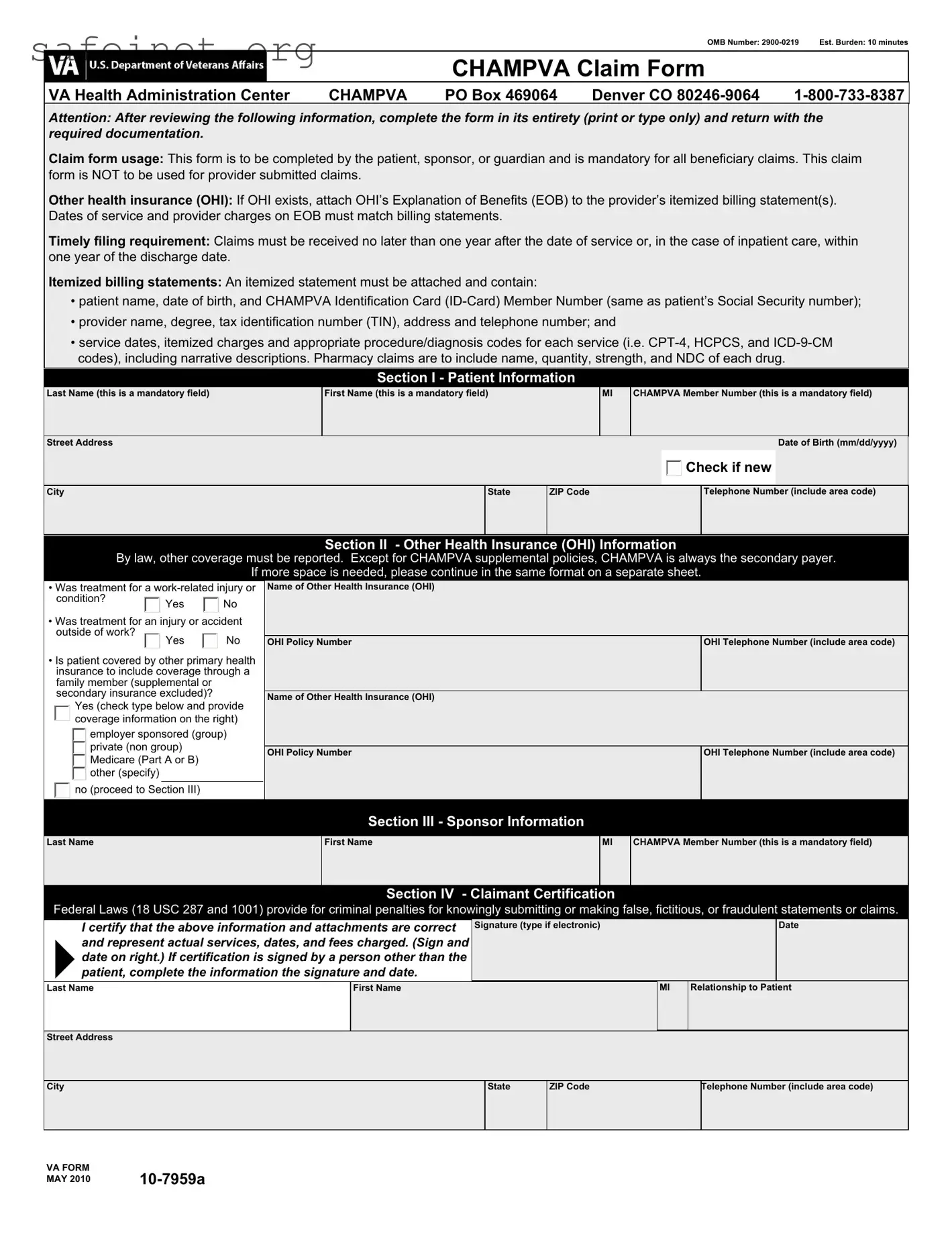
CHAMPVA Claim Form
Notice: Termination of marriage by divorce or annulment to the qualifying sponsor ends CHAMPVA eligibility as of midnight on the effective date of the dissolution of marriage. Changes in status should be reported immediately to CHAMPVA, ATTN: Eligibility Unit, PO Box 469028, Denver, CO 80246-9028 or call 1-800-733-8387.
PRIVACY ACT INFORMATION: The authority for collection of the requested information on this form is 38 U.S.C. 501 and 1781. The purpose of collecting this information is to adjudicate and process claims for CHAMPVA benefits. You do not have to provide the requested information but if any or all of the requested information is not provided, it may delay or result in denial of your request for CHAMPVA benefits. Failure to furnish the requested information will have no adverse impact on any other VA benefit to which you may be entitled. The responses you submit are considered confidential and may be disclosed outside VA only if the disclosure is authorized under the Privacy Act, including the routine uses identified in the VA system of records 54VA16, titled "Health Administration Center Civilian Health and Medical Program Records -VA", as set forth in the Compilation of Privacy Act Issuances via online GPO access at http://www.gpoaccess/privacyact/index.html.For example, information on this form may be disclosed to contractors, trading partners, health care providers and other suppliers of health care services to determine your eligibility for medical benefits and payment for services. Disclosure of Social Security number(s) of those for whom benefits are claimed is requested under the authority of Title 38, U.S.C., and is voluntary. Social Security numbers will be used in the administration of veterans benefits, in the identification of veterans or persons claiming or receiving VA benefits and their records and may be used for other purposes where authorized by Title 38, U.S.C., and the Privacy Act of 1974 (5 U.S.C. 552a) or where required by other statute.
PAPERWORK REDUCTION ACT: This information collection is in accordance with the clearance requirements of Section 3507 of the Paperwork Reduction Act of 1995. Public reporting burden for this collection of information is estimated to average 10 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed and completing and reviewing the collection of information. Comments regarding this burden estimate or any other aspect of this collection, including suggestions for reducing the burden, may be addressed by calling the CHAMPVA Help Line, 1-800-733-8387. Respondents should be aware that notwithstanding any other provision of law, no person shall be subject to any penalty for failing to comply with a collection of information if it does not display a currently valid OMB control number. The purpose of this data collection is to provide a mechanism to claim CHAMPVA benefits.
VA FORM |
10-7959a |
MAY 2010 |
 Check if new
Check if new employer sponsored (group) private (non group)
employer sponsored (group) private (non group) Medicare (Part A or B) other (specify)
Medicare (Part A or B) other (specify)
 no (proceed to Section III)
no (proceed to Section III)